Medication Assisted Treatment (MAT) is a comprehensive, evidence-based approach to overcoming substance use disorders, particularly for opioid and alcohol addiction. It combines FDA-approved medications with counseling and behavioral therapies to treat the whole person, addressing the physical, mental, and emotional aspects of recovery. For those in Massachusetts seeking a path forward, MAT offers a medically sound and supportive framework for building a sustainable, sober future.
Key Takeaways
- MAT is a "Whole-Person" Approach: It combines FDA-approved medications with counseling and therapy to address both the physical cravings and the psychological triggers of addiction.
- It's a Proven Medical Treatment: Recognized as the gold standard for opioid and alcohol use disorders, MAT stabilizes brain chemistry, reduces cravings, and significantly improves survival rates. It is not "trading one drug for another."
- Treatment is Highly Personalized: MAT plans are tailored to individual needs. In Massachusetts, programs like those at South Shore Recovery Center offer different levels of care, from intensive day treatment to flexible outpatient services.
- Support Systems are Crucial: Lasting recovery involves more than just medication. Integrating therapy, dual-diagnosis care for co-occurring mental health conditions, and peer support groups like AA or NA are essential components of a successful MAT program.
A Modern Path to Recovery
When someone is struggling with addiction, it can feel like their brain and body have been hijacked. Medication Assisted Treatment (MAT) is a powerful, evidence-based way to get back in the driver's seat. It’s a comprehensive approach that combines FDA-approved medications with counseling and behavioral therapies.
Think of it as tackling the problem from every angle—addressing the physical, mental, and emotional sides of addiction all at once to build a solid foundation for a new life.
The journey to recovery can seem overwhelming, but modern medicine offers real, tangible hope. MAT provides a structured and supportive path for individuals grappling with opioid or alcohol use disorders. It's crucial to understand this isn't about trading one addiction for another; it's a legitimate medical treatment for what we now know is a chronic brain disease.
The principle behind it is straightforward: addiction physically changes your brain chemistry. MAT uses specific, carefully prescribed medications to help normalize that chemistry. This process reduces the overwhelming cravings and blocks the euphoric effects of alcohol or opioids, giving you the mental space and stability needed to truly engage in therapy and start healing.
Understanding the Treatment Gap
Despite being one of the most effective tools we have against the opioid crisis, far too many people can't access it. In 2022, an estimated 9.367 million U.S. adults needed treatment for an opioid use disorder, but a staggering 25.1% actually received the medications that could help them. This highlights a critical, nationwide gap between the care people need and the care they can get.
Medication Assisted Treatment gives you the stability to step back from the chaos of addiction and start rebuilding your life. It provides the physical support so you can do the mental and emotional work required for true healing.
This integrated approach ensures you're not just managing symptoms but actively building the resilience you need to prevent relapse. To see how these evidence-based programs are structured for positive outcomes, you can discover the benefits of addiction treatment at South Shore Recovery Center.
How MAT Helps the Brain Heal and Rebalance
To really understand what medication-assisted treatment is, you have to see addiction for what it is: a condition that physically changes the brain. Long-term substance use rewires the brain’s circuits for reward, survival, and even decision-making. The brain starts to believe it needs the substance just to feel normal, which kicks off a vicious cycle of intense cravings and debilitating withdrawal.
MAT acts as a kind of lifeline for the brain, giving it the support it needs to heal and find its footing again. These medications aren't a "cure," but they are indispensable tools that stabilize brain chemistry. This stability is what creates the space—the mental clarity and physical relief—for a person to truly engage in therapy and build a solid foundation for recovery.
Rebalancing Brain Chemistry for Opioid Use Disorder
When someone uses opioids, the drugs attach to specific receptors in the brain, unleashing a flood of dopamine that creates a powerful high. Over time, the brain gets used to this and compensates by making less of its own natural "feel-good" chemicals. This is what makes withdrawal so brutal—the brain is suddenly starved of the very chemical it’s learned to depend on.
The medications used for Opioid Use Disorder (OUD) work on these same brain receptors, but in a much more controlled and safer way. Think of it as gently recalibrating the system instead of shocking it.
This visual map shows how the core components of MAT—medication, counseling, and personalized care—work together to support recovery.
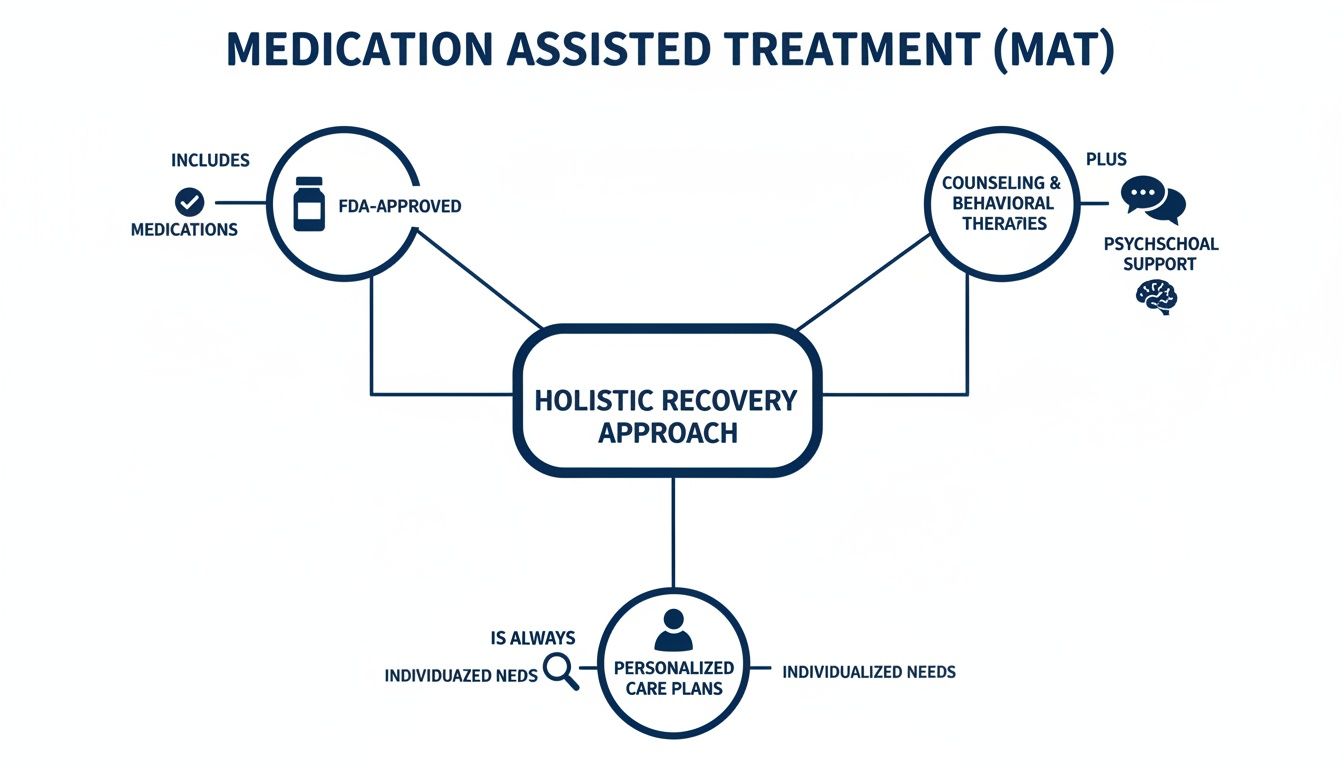
The diagram makes it clear: the medication is just one piece of a comprehensive strategy. It's about treating the whole person, not just the symptoms.
Calming the Brain in Alcohol Use Disorder
Heavy, long-term drinking also wreaks havoc on the brain’s delicate chemical balance, especially with neurotransmitters like GABA (the brain’s brake pedal) and glutamate (the accelerator). The brain gets used to the sedative effect of alcohol and starts pumping out extra glutamate to stay alert. When the drinking stops, this over-excited system can cause severe withdrawal symptoms like intense anxiety, tremors, and insomnia.
Medications for Alcohol Use Disorder (AUD) help bring this system back into equilibrium, easing the transition and making recovery more manageable.
MAT is a legitimate medical treatment, not a substitute addiction. It stabilizes the brain's neurochemistry, providing a platform from which individuals can build sustainable recovery skills and reclaim their lives.
For instance, acamprosate helps rebalance the GABA and glutamate systems, which reduces those nagging, uncomfortable symptoms of post-acute withdrawal that can linger for months. By easing that distress, it significantly lowers the risk of relapse. Another medication, disulfiram, takes a different approach by creating a very unpleasant physical reaction to alcohol, which acts as a strong deterrent.
To give you a clearer picture, here’s a breakdown of the most common medications used in MAT for both opioid and alcohol use disorders.
Common MAT Medications and How They Work
| Medication | Used For | How It Works |
|---|---|---|
| Buprenorphine (Suboxone®) | Opioid Use Disorder (OUD) | A partial opioid agonist. It binds to opioid receptors to reduce cravings and prevent withdrawal but has a "ceiling effect" to prevent a high. |
| Naltrexone (Vivitrol®) | Opioid & Alcohol Use Disorders | An antagonist. It blocks the euphoric effects of opioids and can reduce cravings for alcohol, removing the "reward" from substance use. |
| Methadone | Opioid Use Disorder (OUD) | A full opioid agonist. It activates opioid receptors to relieve withdrawal and cravings, administered in a controlled clinical setting. |
| Acamprosate | Alcohol Use Disorder (AUD) | Helps restore the balance between GABA and glutamate neurotransmitter systems, easing post-acute withdrawal symptoms like anxiety and restlessness. |
| Disulfiram | Alcohol Use Disorder (AUD) | Creates an unpleasant physical reaction (nausea, headache) if alcohol is consumed, acting as a powerful deterrent against drinking. |
Each of these medications works on a different biological pathway, but the goal is the same: to give the brain the stability it needs to heal.
Dismantling the Myth of "Trading One Drug for Another"
One of the most persistent and damaging myths about MAT is that it’s just swapping one addiction for another. This couldn't be further from the truth.
These are FDA-approved medications prescribed and monitored by medical professionals. The doses are carefully managed to normalize brain function, not to create a high. When used correctly, these medications don't impair someone's ability to think clearly, go to work, or be present for their family.
Instead, they provide the biological foundation needed for a person to truly benefit from counseling, mend relationships, and start rebuilding their life. For so many people in Massachusetts, this treatment is the key that finally unlocks the door to a lasting recovery.
Combining Medication With Therapy for Lasting Change
Medication can be a game-changer for stabilizing the brain during early recovery, but it’s only one piece of the puzzle. Real, sustainable change comes from looking at the whole person, which means pairing Medication-Assisted Treatment with dedicated counseling and behavioral therapies.
Think of it like this: medication lays a new, stable foundation for a house that's been shaken. But therapy is the crucial work of rebuilding the rooms, reinforcing the walls, and making it a place you actually want to live in again.
This combination is absolutely essential for long-term success. While the medication gets to work on the biology of addiction—quieting the constant cravings and taking the edge off withdrawal—therapy gets to the psychological heart of the matter. It's in those sessions that you begin to understand why you turned to substances and start building the skills to live a full life without them.

Uncovering the Roots With Proven Therapies
Evidence-based therapies are what help you move from simply managing addiction to truly healing from it. Two of the most effective approaches used alongside MAT are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Cognitive Behavioral Therapy (CBT): This is all about learning to connect the dots between your thoughts, feelings, and actions. CBT helps you identify those automatic, destructive thinking patterns that lead to substance use and gives you practical ways to challenge and change them.
- Dialectical Behavior Therapy (DBT): DBT is particularly powerful for anyone who feels overwhelmed by intense emotions. It teaches concrete skills for mindfulness, emotional regulation, and distress tolerance, giving you a new playbook for coping with life’s stressors.
These aren't just abstract concepts; they are practical tools for real-world challenges. To get a better sense of how these patterns are rewired, you can learn more about Cognitive Behavioral Therapy in our detailed guide.
The Critical Role of Dual-Diagnosis Care
It is incredibly common for a substance use disorder to walk hand-in-hand with another mental health condition, like anxiety, depression, or PTSD. When they exist together, it’s called a dual diagnosis. Trying to treat the addiction without addressing the underlying mental health issue is like bailing water out of a boat but never patching the hole.
Any effective MAT program will screen for and treat these co-occurring conditions right from the start. For example, someone may have started using opioids to numb the feelings of chronic anxiety. A dual-diagnosis approach gives them medication to manage their SUD while also providing targeted therapy and, if needed, medication for their anxiety. This ensures every aspect of a person’s well-being is cared for, which dramatically increases the odds of a successful recovery.
"True recovery isn’t just about stopping substance use; it’s about building a life you don’t feel the need to escape from. Therapy provides the blueprint for that new life."
This integrated method is the gold standard of care for a reason. It acknowledges that mental health and addiction are deeply intertwined, and by treating both at the same time, we build a much stronger, more resilient foundation for the future.
The South Shore Recovery Center Model
Here at South Shore Recovery Center, our programs are designed to show how all these moving parts work together in harmony. A client's journey with us isn't just about picking up a prescription. It's about stepping into a structured and supportive environment where every part of their healing is connected.
A typical day might involve:
- Medical Check-ins: To make sure the medication is working as it should and to manage any side effects.
- Individual Therapy: Private, one-on-one sessions to work through personal history, trauma, and triggers.
- Group Counseling: Peer-supported discussions that foster a sense of community, fight isolation, and allow for shared learning.
This combination creates a powerful synergy. The medication provides the physical and mental stability needed to engage, while individual and group therapy provide the emotional tools and human support to build a new life. It’s this complete, wrap-around approach that helps turn the desire for sobriety into a sustainable reality. And this model's effectiveness is being recognized globally; the medication-assisted treatment market is projected to grow by over 8.8% annually as more people seek out this comprehensive care.
Finding a MAT Program in Massachusetts
It’s one thing to know that real, effective help is out there. It’s another thing entirely to know how to find it. If you’re in Massachusetts, the good news is that starting a MAT program is a clear, manageable step you can take today. From the moment you pick up the phone, the process is built around confidentiality and support, making sure you feel heard and respected.
Taking that first step isn't about making a huge commitment right away—it starts with a simple conversation. At a place like South Shore Recovery Center in Plymouth, MA, it all begins with an initial assessment. This isn’t some high-pressure test; it's a genuine conversation where a clinical expert takes the time to listen to your story, understand your medical background, and hear what you want to achieve in recovery. This first meeting lays the foundation for your entire treatment plan.

What to Expect on Your Treatment Journey
That initial assessment is used to build a treatment plan that's all about you. It's not a rigid, one-size-fits-all program. Instead, it’s flexible, meeting you exactly where you are with different levels of care to match what you need right now.
Most people start with more intensive support to get stable, then gradually move to less frequent care as they gain new skills and confidence. This "step-down" approach is common in outpatient treatment and ensures you’re never overwhelmed or left without enough support.
- Day Treatment Programs (PHP): This is the highest level of outpatient support. You'll typically spend several hours a day in treatment, five days a week, giving you a strong, structured environment while still letting you go home at night.
- Intensive Outpatient Programs (IOP): One step down from PHP, IOP offers a great balance of structure and personal freedom. Treatment usually happens for a few hours a day, a few times a week, so you can more easily manage work, school, or family life.
- Outpatient Programs (OP): This is the most flexible level, often involving weekly therapy sessions. It’s a perfect fit for people who have built a solid recovery foundation and just need that consistent support to keep moving forward.
As you make progress, your plan changes with you. You can learn more about how these levels fit together by exploring different opioid addiction treatment options.
Navigating Insurance and Coverage
Worrying about how to pay for treatment is completely normal, but it shouldn't stop you from getting help. The great news is that because MAT is recognized as a vital, evidence-based medical treatment, most major insurance plans in Massachusetts provide coverage.
Figuring out your insurance benefits shouldn't be another roadblock. A good treatment center will have staff who can take care of all of that for you.
When you call a center like South Shore Recovery Center, an admissions coordinator can check your insurance benefits on the spot, often in just a few minutes. They’ll break down your coverage in simple terms so you know exactly what’s what. This takes the stress and guesswork out of the equation, letting you focus on what really matters—your health.
Taking That First Actionable Step
It takes incredible strength to reach out for help. We know it can feel like a huge hurdle, so the process is designed to be as straightforward and painless as possible. Here’s how you can start today:
- Make a Confidential Call: Just pick up the phone. You'll speak with an admissions specialist who is there to answer your questions—with no judgment—and walk you through what comes next.
- Have Your Info Ready: To make things go smoothly, try to have your insurance card nearby. It also helps to be ready to share a little bit about your history with substance use.
- Schedule Your Assessment: The final piece is setting a time for your initial assessment. This meeting is your official starting line on the path to a healthier, more meaningful life.
For anyone on the South Shore or across Massachusetts, high-quality, compassionate MAT is closer than you think. One confidential phone call is all it takes to start taking back your future.
Let's Clear Up Some Common Myths About MAT
Misinformation about Medication-Assisted Treatment is a huge problem. It builds walls of fear and stigma, stopping people from getting help that could genuinely save their lives. It's frustrating to see these myths persist, especially when they paint such a wrong picture of what MAT actually is and how it helps people.
It’s time to set the record straight. By tackling these false beliefs with facts, we can help individuals and their families here in Massachusetts feel confident enough to choose a path based on solid science, not outdated fears.
Myth 1: "You're Just Trading One Drug for Another."
This is probably the most common and damaging myth out there. The idea that medications like buprenorphine or naltrexone are just "substitutes" for street drugs couldn't be more wrong. These are FDA-approved medications, prescribed and managed by doctors in a safe, clinical environment.
Unlike illicit drugs, these medications don't get you "high" when you take them as directed. Their job is to restore balance to your brain chemistry. They quiet the relentless cravings and can even block the euphoric rush from opioids or alcohol, which removes the incentive to use. This medical oversight is the critical difference between addiction and treatment—it gives you the biological stability you need to even begin the work of recovery.
Myth 2: "It's Not 'Real' Recovery."
Some people hold the belief that the only "true" recovery is one based on complete abstinence, without any medication at all. This perspective usually comes from a fundamental misunderstanding of addiction. Addiction isn't a moral failure; it's a chronic, relapsing brain disease. Using MAT is no different than a person with diabetes using insulin or someone with heart disease taking blood pressure medication. It's a medical tool for a medical condition.
Recovery is all about getting your health back, rebuilding your life, and finding purpose again. For so many people, MAT is the very thing that makes all of that possible. In fact, the World Health Organization backs this approach, citing it as the single most effective intervention we have. It leads to less substance use, lower death rates, and a much better quality of life. You can discover more about the life-saving impact of MAT on drugabusestatistics.org.
MAT is a long-term strategy for managing a chronic health condition. It provides the stability needed to address the root causes of addiction through therapy, rebuild relationships, and develop the skills for a sustainable, sober life.
Ultimately, it’s about using every proven tool in the toolbox to heal.
Myth 3: "It's Just a Short-Term Crutch."
Another misconception is that MAT is just a quick fix to get through the misery of withdrawal. While it is incredibly helpful for managing that initial, acute phase, its real power often lies in long-term recovery support. Addiction physically changes the brain, and healing from those changes takes time.
Many people find that staying on their medication for months, or even years, provides the steady support they need to keep relapse at bay. There is no predetermined timeline. How long someone stays on MAT is a clinical decision made between them and their doctor, based entirely on their unique needs and progress. The goal is always lasting wellness, not a temporary patch.
Myth 4: "The Medication Will Make You Unable to Function."
It's completely normal to have questions about side effects, but the fear that MAT medications will leave you groggy or impaired just isn't true. When prescribed and dosed correctly, these medications are designed to do the exact opposite. They help people get back to their lives—to work a job, take care of their kids, and be a part of their community again.
Your medical team will work closely with you, monitoring how you're doing and adjusting your dosage to make sure you get the most benefit with the fewest side effects. It's a carefully managed process focused on your safety and well-being. Far from holding you back, MAT is what gives many people the clarity and stability they need to fully show up for their new, healthier life.
Frequently Asked Questions About Medication-Assisted Treatment
Deciding to get help for a substance use disorder is a huge, courageous step. But it's also completely normal to have a lot of questions about what comes next, especially when it comes to Medication-Assisted Treatment (MAT). To help clear things up, here are answers to some of the most common questions we hear from individuals and families across Massachusetts.
How long does medication-assisted treatment last?
There is no set timeline for MAT. Treatment length is highly individualized and depends on your personal progress and clinical needs. Some people use MAT for several months to build a foundation in early recovery, while others may continue for several years to manage what is often a chronic condition. The decision to adjust or taper off medication is made collaboratively between you and your medical team.
Can I participate in 12-step groups like AA or NA while in a MAT program?
Yes, absolutely. We strongly encourage combining the medical support of MAT with the peer fellowship of groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). This creates a well-rounded recovery plan that addresses both the physical and the psychosocial aspects of healing. While some individual meetings may hold outdated views, the official stance of these organizations supports members regardless of their medical choices.
How do I know if MAT is the right choice for me?
The best way to determine if MAT is a good fit is through a professional assessment. When you contact a treatment center like South Shore Recovery in Plymouth, MA, the first step is a confidential evaluation. A clinical expert will discuss your substance use history, medical background, and recovery goals to recommend the most appropriate treatment options, ensuring you can make an informed and empowered decision.
What is the role of family in the MAT process?
Family plays a vital role in recovery. Addiction impacts the entire family system, which is why comprehensive MAT programs include family therapy and education. At South Shore Recovery Center, we work with your loved ones to help them understand the science of addiction, learn how to provide effective support, and rebuild healthy communication. An informed and engaged family becomes a powerful support network for long-term success.
