Cognitive Behavioral Therapy, or CBT, is a practical, evidence-based form of psychotherapy that helps people understand the powerful connection between their thoughts, feelings, and behaviors. It provides the tools to identify and challenge negative thinking patterns, empowering individuals across Massachusetts to build healthier coping skills for life's challenges, from anxiety and depression to substance use disorders.
Key Takeaways
- CBT focuses on the present: Unlike therapies that delve deep into the past, CBT addresses current problems by teaching you to challenge the negative thought cycles happening right now.
- Thoughts, feelings, and actions are linked: The core of CBT is the "cognitive triangle," which shows how your thoughts directly influence your emotions and behaviors. By changing your thoughts, you can change your reality.
- It's a skills-based therapy: CBT is active and hands-on. You'll learn practical techniques like cognitive restructuring and behavioral activation to manage your mental health proactively.
- It is highly effective for addiction: CBT is a cornerstone of modern addiction treatment, providing proven strategies to identify triggers, manage cravings, and build a resilient recovery.
So, What Exactly Is Cognitive Behavioral Therapy?
Many forms of therapy spend a lot of time digging into your past to understand why you are the way you are. While that can be valuable, CBT focuses on the here and now. It’s less about why the problems started and more about giving you the tools to solve them today.
I like to use a garden analogy. Imagine your mind is a garden where negative thought patterns are like weeds. They pop up, they’re persistent, and they can easily choke out the healthy plants—your positive emotions and constructive behaviors. CBT doesn't just rip out the weeds for you. Instead, it teaches you how to become a skilled gardener of your own mind. You learn to spot the weeds as they appear, understand the conditions that help them grow, and actively cultivate a healthier, more resilient inner landscape. This is why it's so empowering; you're building skills for life.
This entire framework has its roots in the 1960s with psychiatrist Aaron Beck. He realized that our internal monologue—those automatic thoughts that run through our heads—has a massive impact on our emotional state. By challenging and changing those distorted thoughts, we can fundamentally alter how we feel and act. You can learn more about the foundational principles of CBT to see just how deep its impact has been.
This focus on practical, lasting change is what makes CBT one of the most respected and effective therapies available today. It’s a collaborative journey between you and your therapist, building a structured path toward a healthier, more resilient you.
Understanding How Your Thoughts Shape Your Reality
Cognitive Behavioral Therapy is built on a deceptively simple idea: it's not the events in our lives that cause our feelings, but how we think about those events. This is the whole game. Once you grasp this, you can start to see how much power you have to change your own experience.
Let's use a real-world example. Imagine you’re driving down I-93 in Boston and another car suddenly cuts you off.
One person’s instant thought might be, "What a jerk! They could have killed me!" That thought immediately sparks anger and frustration. Their heart might pound, their knuckles turn white on the steering wheel, and they might lay on the horn or tailgate the other car.
Now, picture another person in the very same situation. Their thought might be, "Whoa, they must be in a serious rush. Maybe it's an emergency." This interpretation leads to a completely different emotional response—maybe a flicker of concern, or even just indifference. They simply take their foot off the gas, let the other car go, and continue on with their day, unbothered.
Same event, two completely different realities. The only thing that changed was the thought process.
The Cognitive Triangle: The Core of CBT
This powerful link between what we think, how we feel, and what we do is what therapists call the Cognitive Triangle. Think of it as a constant feedback loop. Your thoughts influence your emotions, your emotions drive your physical sensations and actions, and those actions then reinforce your original thoughts.
It's a cycle. A negative thought can kick off a cascade of difficult feelings, which can then push you toward self-defeating behaviors. Before you know it, you're stuck in a loop that seems impossible to break.
This is what that cycle looks like in action:
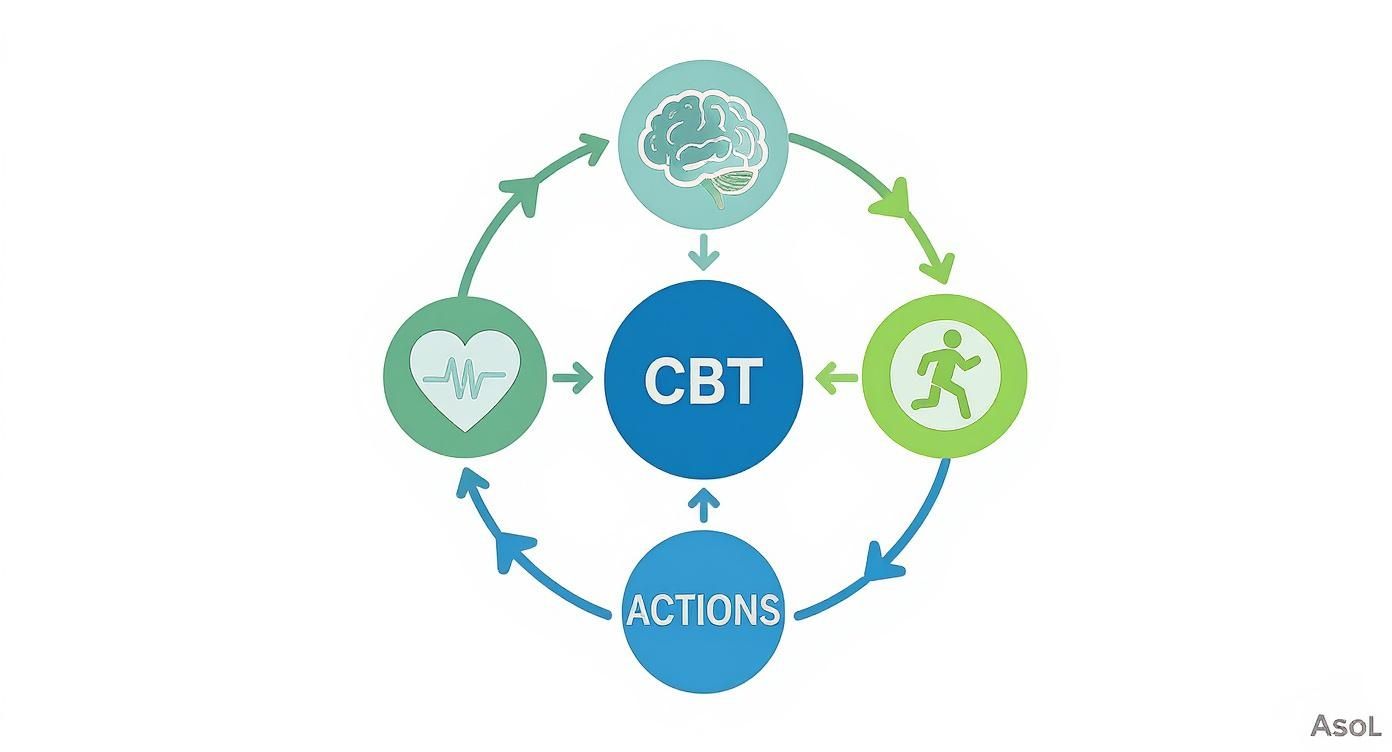
The goal of CBT isn't to stop having thoughts or feelings. It's about learning how to step into that cycle and nudge it in a healthier direction.
Automatic Negative Thoughts and Cognitive Distortions
So where do these unhelpful thoughts come from? Often, they are Automatic Negative Thoughts—or ANTs, a fitting acronym. These are knee-jerk reactions that flash through our minds so quickly we don't even question them. They feel like objective truth, but more often than not, they’re just old, well-worn mental habits.
These ANTs are usually products of cognitive distortions, which are essentially flawed patterns of thinking that color our reality in a negative light. They're like looking at the world through a warped, funhouse mirror.
Cognitive distortions aren't a sign that you're "broken." They are common mental shortcuts everyone takes. The problem is that for many of us, these shortcuts consistently lead to a dead end of anxiety, depression, and self-sabotage.
A classic example is "all-or-nothing thinking." Someone in recovery might have a single drink after months of sobriety and immediately think, "I've completely blown it. I'm a total failure, and my recovery is over." This black-and-white thinking completely discounts all the progress made and can create such a strong feeling of hopelessness that it actually triggers a full-blown relapse.
Here are a few other common thinking traps you might recognize:
- Mind Reading: You're convinced you know what someone else is thinking (and it's usually negative). "My therapist was quiet today. He must think I'm not making any progress."
- Catastrophizing: You automatically jump to the worst-possible conclusion. "I felt a craving today. This means I'm going to relapse for sure and lose my job and my family."
- Personalization: You take the blame for things that have little or nothing to do with you. "My son got a bad grade on his test. I must be a terrible parent."
Simply learning to spot these distortions is the first, massive step. When you can label a thought—"Oh, that's catastrophizing again"—you rob it of its authority. It stops being a "fact" and becomes just a thought, one that you have the power to challenge and change. This is where the real work, and the real healing, begins.
Putting CBT Into Practice With Proven Techniques
Cognitive Behavioral Therapy isn't just a bunch of theories; it's an active, hands-on therapy defined by its powerful techniques. These are the tools that let you become a direct participant in your own recovery. Instead of just talking about problems, you and your therapist roll up your sleeves and build a practical skill set you can use for the rest of your life.
These methods are specifically designed to break the cycle of negative thoughts, feelings, and behaviors we talked about earlier. They give you a structured way to confront unhelpful thinking and build healthier habits, one step at a time. The real goal here is to move from simply being aware of a problem to actively doing something about it.

A Quick Look at Common CBT Techniques
To give you a clearer picture, here’s a breakdown of some of the most common tools a CBT therapist might use. Think of this as a look inside the CBT toolbox.
| Technique | Primary Purpose | Example Application |
|---|---|---|
| Cognitive Restructuring | Identifying and challenging irrational or unhelpful thoughts. | Questioning the thought "I'm a total failure" after a single mistake by looking for evidence of past successes. |
| Behavioral Activation | Re-engaging in positive activities to combat depression and avoidance. | Scheduling a 15-minute walk, even when you don't feel like it, to prove that action can improve mood. |
| Journaling/Thought Records | Tracking thoughts, feelings, and behaviors to identify patterns. | Writing down a situation that caused anxiety, the automatic thought, and the emotional response to analyze later. |
| Exposure Therapy | Gradually facing feared situations to reduce anxiety and phobias. | For a social phobia, practicing making small talk with a cashier under a therapist's guidance. |
Each of these techniques empowers you to take control, providing concrete steps you can take to change your mental and emotional state. Let's dig a little deeper into a few of the most foundational ones.
Unpacking Your Thoughts With Cognitive Restructuring
One of the cornerstones of CBT is cognitive restructuring. This is essentially the process of identifying, challenging, and reframing your automatic negative thoughts (ANTs). You learn to act like a detective for your own mind, searching for real evidence that either supports or refutes your most distressing thoughts.
Your therapist guides you in learning how to question these thoughts instead of just accepting them as fact. For instance, if you make a mistake at work, an automatic thought might scream, "I'm so incompetent."
Cognitive restructuring teaches you to pause and ask some tough questions:
- What's the evidence? "Okay, I made one mistake. But I've also successfully completed dozens of projects. Does this one slip-up really define my entire competence?"
- Is there another way to see this? "Maybe this was just a simple error that anyone could make, not a reflection of a deep personal failing."
- What's the worst that could happen, and can I handle it? "My boss might point it out. I can take the feedback, fix the issue, and learn from it. I'll survive."
This process isn't about slapping a layer of fake "positive thinking" on top of your problems. It’s about cultivating a more balanced, realistic, and fair perspective. With practice, you start to loosen the grip these negative thought patterns have on your emotions and actions.
Reconnecting With Your Life Through Behavioral Activation
When you're struggling with something like depression or substance use, it's incredibly common to pull back from activities that once brought you joy and a sense of purpose. Behavioral Activation is a powerful technique designed to reverse that trend by helping you gradually re-engage with positive, rewarding experiences.
The principle is brilliantly simple: action can change your mood. Just waiting around to feel motivated almost never works. Instead, you and your therapist schedule meaningful activities and you commit to doing them, even if you don't feel like it in the moment.
For someone in early recovery in a Massachusetts town, this might look like:
- Start Small: Forget a marathon. Maybe it’s just a 10-minute walk along Plymouth Harbor.
- Schedule It: You put it in your calendar, treating it with the same importance as a doctor's appointment.
- Track Your Mood: You take a moment to notice how you feel before, during, and after the walk.
These small actions build momentum over time. They provide your brain with positive reinforcement, lift your mood, and fight back against the inertia of depression and addiction. It's about rebuilding a life that feels rich with meaning. This proactive strategy is often paired with other therapies to boost commitment; you can find out more about that in our guide on what is motivational interviewing therapy.
The core idea of Behavioral Activation is that by changing what you do, you can directly influence how you feel. It’s a proactive strategy for breaking the cycle of avoidance and isolation.
Why CBT Is a Cornerstone of Modern Addiction Treatment
When it comes to treating substance use disorders, Cognitive Behavioral Therapy isn't just another tool in the toolbox—it's a foundational, evidence-based approach that truly works. Its power comes from giving you a clear, logical roadmap for recovery. Instead of getting stuck on the behavior of using, CBT goes deeper to target the root cause: the thoughts and beliefs that keep the cycle of addiction going.
For anyone in Massachusetts struggling with addiction, this therapy offers the real-world skills needed to navigate the tough moments of sobriety. It’s all about empowering you to spot your personal triggers, challenge the destructive thinking that keeps you stuck, and build healthier coping skills that prevent relapse for good.
1. Identifying and Managing Personal Triggers
The first real step toward recovery is understanding what pulls you back toward substance use. We call these "triggers"—the specific people, places, feelings, or situations that ignite cravings. CBT gives you a structured way to pinpoint these high-risk scenarios with incredible precision.
Through guided self-monitoring exercises, like journaling, you start to see the patterns. You connect the dots between the thoughts and feelings that come right before a craving hits. For example, you might realize that the feeling of loneliness on a Friday night is a massive trigger. Once you know that, you can create a proactive plan to handle that exact situation, turning a moment of weakness into a chance to build strength. This is a critical process we break down in our guide to CBT for addressing cravings and triggers.
2. Challenging the Thoughts That Fuel Addiction
Let’s be honest: addiction is often propped up by a powerful inner voice filled with what we call cognitive distortions. These are basically faulty, unhelpful ways of thinking that make using substances seem like a good idea.
Sound familiar?
- "I've had a brutal week, I deserve this." (Justifying)
- "Just one won't hurt anything." (Minimizing the consequences)
- "There's no way I can handle this stress without it." (Catastrophizing)
CBT teaches you, step-by-step, how to take these thoughts apart. You learn to stop treating them as facts and start seeing them for what they are: ideas that can be questioned and challenged. By looking for the actual evidence behind these beliefs, you can start forming more balanced, realistic responses that strip them of their power over your actions.
The core idea is simple but life-changing: if you can change your thinking, you can change your behavior. CBT gives you the tools to systematically dismantle the very thoughts that keep the addiction cycle spinning.
3. Building Resilient Coping Skills for Sobriety
Lasting recovery isn't just about stopping substance use. It's about what you do instead. You have to replace those old, destructive habits with new, healthy ones. This is where CBT truly shines—it helps you build a solid toolkit of practical coping skills you can pull out and use the moment a craving or a difficult emotion shows up.
And we're not just talking about simple distraction. These are specific, actionable strategies for managing stress, handling emotions, and solving problems without turning back to old habits. Over time, these skills become your new go-to responses, building the kind of resilience and self-confidence that lasts.
4. A Proven Track Record of Success
CBT isn't some new-age trend; it's one of the most thoroughly researched therapies for addiction, with decades of scientific studies backing it up. Its success isn't just a collection of stories—it's supported by hard data showing its power to create lasting change.
For instance, extensive research shows just how effective this approach can be. Studies have found that around 61.38% of patients achieve remission immediately after finishing CBT treatment. That number often climbs to nearly 75% at the six-month follow-up, which shows that the skills you learn actually get stronger with practice. You can explore more detailed CBT success rates to see the long-term proof for yourself.
This is exactly why top-tier facilities, including our outpatient programs here in Massachusetts, make CBT a core part of their treatment plans. It provides a reliable, structured path toward not just getting sober, but achieving genuine, sustained well-being.
Navigating Your First CBT Program in Massachusetts
Deciding to start therapy is a big deal, and it's totally normal to feel a little uncertain about what comes next. Knowing what to expect when you join a Cognitive Behavioral Therapy program—especially one right here in Massachusetts—can make the whole process feel much less intimidating. Think of it as a structured, collaborative journey designed to put you firmly in the driver's seat of your own recovery.
It all kicks off with an open conversation. That first step isn’t about being put on the spot; it’s about sharing your story in a safe, completely non-judgmental space.

Your Initial Assessment
The very first meeting is your initial assessment. This is dedicated time for your therapist to really get to know you and understand your unique situation. You’ll talk through the specific challenges you're facing—whether that’s substance use, anxiety, or both—and what you want to change. This conversation lays the foundation for your personalized treatment plan, making sure the therapy is perfectly aligned with your needs from day one.
Collaborating on Your Goals
Right after the assessment, you and your therapist will sit down together to set concrete, measurable goals. This isn't a vague "I want to feel better" kind of discussion. It’s about defining what "better" actually looks like for you.
For instance, a goal might be something like: "To reduce my social anxiety so I can attend family gatherings without needing a drink," or "To develop three healthy coping strategies I can use the moment I feel a craving." These clear targets give your therapy real direction and make it much easier to see and track your progress along the way.
The Structure of a Typical Session
CBT sessions are active and have a predictable structure, which helps make the process feel organized and productive.
A typical session is a partnership. It’s a space to check in on progress, set a clear agenda for the day's work, and actively practice the new cognitive and behavioral skills you're learning.
A session often starts with a quick check-in on your week and a review of any "homework" or skills you might have practiced. From there, you and your therapist set an agenda for the day, focusing on a specific problem or skill. The majority of the time is spent learning and applying CBT techniques, and it wraps up by creating a plan for you to practice those skills in the week ahead. This reliable structure ensures every single session builds momentum toward your goals.
Where CBT is Headed: Therapy in a Modern World
Cognitive Behavioral Therapy isn't some old-school approach stuck in the past. It's constantly evolving to fit the way we live now. With the rise of telehealth and mental health apps, high-quality CBT is becoming more accessible than ever, especially for people here in Massachusetts who might struggle with travel or packed schedules.
This evolution shows that CBT isn't just a proven therapy; it's a living, breathing field that keeps growing. The goal is simple: make sure more people can get the effective treatment they deserve, whether that’s in a therapist’s office or through a screen.
More People Are Seeking CBT Than Ever Before
As the stigma around mental health slowly fades, the demand for therapies that actually work—like CBT—has skyrocketed. You don't have to take my word for it; just look at the numbers.
The global market for Cognitive Behavioral Therapy is a perfect example. It was valued at around USD 7.51 billion in 2025 and is expected to climb to an incredible USD 21.62 billion by 2031. That's not just a small jump. This growth is being driven by a worldwide recognition of mental health needs, and North America makes up over 32% of that market. You can read more about this expanding CBT market and see the data for yourself.
This isn't just about business; it’s a clear signal that we're finally starting to prioritize mental wellness on a global scale. It means that effective, evidence-based care is becoming a real, reachable option for more and more people.
Common Questions About Cognitive Behavioral Therapy
How long does CBT take to work?
There's no magic number, but most people start to see and feel significant changes within 12 to 20 sessions. The real beauty of CBT is that it’s all about teaching you skills you can start using immediately, which is why progress can often feel quicker than with other types of therapy.
Is CBT covered by insurance in Massachusetts?
Yes, the vast majority of major insurance plans in Massachusetts cover CBT. Because it's a well-respected and evidence-based treatment for so many conditions, it’s considered a standard of care. That said, it's always a good idea to give your insurance provider a quick call to confirm the specifics of your plan.
What makes CBT different from other therapies?
The biggest difference is its structure and focus. CBT is very much about solving the problems you're facing right now. While some therapies might spend a lot of time exploring your distant past, CBT hones in on the present moment. It shares some common ground with other therapies, and you can learn more about one of its offshoots by reading our guide on what is dialectical behavior therapy.
Do I have to do 'homework' in CBT?
Yes, and this is where the real change happens! Practicing the skills you learn in your sessions is a fundamental part of CBT. This "homework" isn't like schoolwork; it's about applying what you're learning to your actual life. It might involve things like jotting down your thoughts in a journal or consciously challenging a negative belief as it pops up during your day. This practice is what turns therapy insights into lasting, real-world change.
How does CBT specifically help with relapse prevention?
CBT helps you look ahead to anticipate high-risk situations before they happen. You'll work with your therapist to rehearse how you'll handle those moments. By having a clear plan for what to do when a trigger appears, you're far less likely to be blindsided and can navigate the challenge without falling back on substance use.
Is CBT effective for co-occurring disorders like anxiety and addiction?
Absolutely. In fact, CBT is a leading treatment for both anxiety and substance use. It’s highly effective because it targets the underlying thought patterns—like constant worry and worst-case-scenario thinking—that fuel both conditions. This makes it an ideal therapy for anyone in Massachusetts dealing with a dual diagnosis.
