Living with bipolar disorder is challenging enough, but when combined with substance abuse, it creates a complex dual diagnosis that can feel overwhelming. This guide breaks down the connection between these two conditions, why integrated treatment is crucial, and how to find effective, compassionate care right here in Massachusetts.
Key Takeaways
- High Co-occurrence: Nearly 56% of individuals with bipolar disorder will also experience a substance use disorder, often starting as an attempt to self-medicate intense mood swings.
- Integrated Treatment is Essential: The most effective approach is integrated care, where mental health and addiction are treated simultaneously by one cohesive team. This is the gold standard for long-term recovery.
- Local Massachusetts Programs: Structured outpatient programs like Partial Hospitalization (PHP) and Intensive Outpatient (IOP) provide expert dual diagnosis care without requiring you to leave your community.
- Aftercare is Crucial: Lasting recovery depends on a strong aftercare plan that includes relapse prevention strategies, peer support groups (like DBSA Massachusetts), and continued professional guidance.
Why Do Bipolar Disorder and Substance Abuse Overlap So Often?
For many, using alcohol or drugs feels like a solution to manage the unpredictable nature of bipolar disorder. Someone might drink to quiet the racing thoughts of a manic episode or use a sedative to escape the despair of a depressive phase. This creates a vicious cycle where the "solution" becomes a second, equally serious problem.
The Role of Behavior and Biology
During a manic phase, impulsivity is dialed way up. This can lead to risky behaviors like binge drinking or experimenting with stimulants without a second thought. On the flip side, a depressive episode can make substances seem like the only escape from emotional pain, which only deepens feelings of isolation.
It's a powerful combination of factors at play:
- Self-medication to try and level out intense moods.
- Loss of impulse control during mania.
- Shared genetic vulnerabilities and brain chemistry.
- Environmental triggers and stressors common in our Massachusetts communities.
This pattern of self-medication and impulsivity is what often fuels the tangled cycle of addiction and mood instability, making both conditions harder to manage.
The connection goes deeper than just behavior. Scientists have found overlapping genetic markers that can predispose someone to both a mood disorder and a substance use disorder. The same neurotransmitter imbalances that contribute to bipolar symptoms can also make a person more vulnerable to addiction.
This is why treating just one condition while ignoring the other rarely works. An addiction program that doesn't include psychiatric care for bipolar disorder is likely to see high relapse rates. True, lasting recovery requires a specialized approach that understands how these two conditions feed each other.
If you want to understand more about how these conditions interact, our guide on treating co-occurring mental health and substance use disorders is a great place to start.
What This Means For Treatment
For anyone in Massachusetts struggling with this dual diagnosis, recognizing the connection is the first critical step. The most effective approach, and the one we champion on the South Shore, is integrated care. This means a single, comprehensive assessment that looks at both your mood patterns and substance use at the same time.
Coordinating care this way ensures nothing falls through the cracks. It sets the stage for a treatment plan that addresses the whole person, not just one set of symptoms.
How Substance Use Complicates Bipolar Symptoms
Balancing bipolar disorder feels like walking a tightrope every day. Introducing drugs or alcohol is the equivalent of tossing pebbles onto that rope—suddenly, what was a careful stride becomes unstable and risky.
Worldwide, about 37 million people live with bipolar disorder. Once substance use enters the equation, mood swings intensify, treatment hits more obstacles, and suicide risk climbs. Understanding why these two conditions amplify each other is a vital first step.
Igniting Mania And Deepening Depression
No two substances impact bipolar disorder in the same way. In fact, the kind of drug or alcohol changes the dynamic entirely.
- Stimulants (cocaine, amphetamines) can trigger manic or hypomanic states—think of lighting a fuse on already volatile energy and racing thoughts.
- Depressants (alcohol, opioids) often offer a false calm. Though someone might reach for them to numb anxiety or pain, they tend to drag mood into a deeper, more persistent depression.
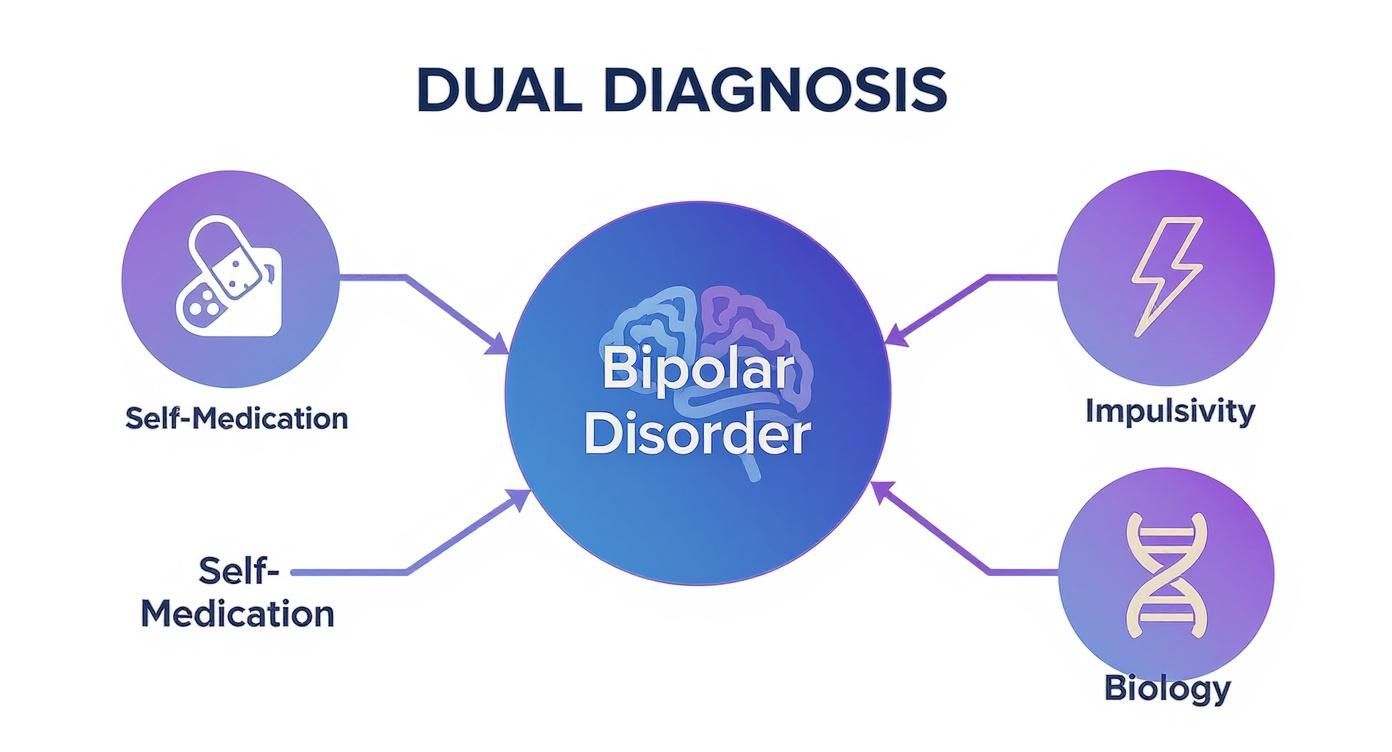
The graphic lays out how self-medication, impulsive habits, and shared biological factors form a feedback loop that’s hard to break.
Sabotaging Treatment And Medication
Perhaps the most critical challenge is how substances interfere with prescribed psychiatric drugs. Stabilizers like lithium or anticonvulsants need steady levels in your system to work properly.
Substance use disrupts this balance by:
- Altering Medication Metabolism: Alcohol and certain drugs can speed up or slow down how the liver processes mood stabilizers, leading to either reduced effect or toxic build-up.
- Masking Symptoms: When substance effects mimic mood swings, it’s tougher for clinicians to pinpoint the root issue, causing misadjusted dosages.
- Reducing Adherence: Active addiction often leads to missed or skipped doses, which can send mood states careening out of control.
When drugs or alcohol enter the picture, the entire foundation of bipolar treatment tilts. Frequent hospital visits and a steep drop in overall health often follow.
This reality underlines why an integrated, dual-diagnosis strategy—tackling both bipolar symptoms and substance use at once—is non-negotiable for lasting recovery. Treating one without addressing the other is like fixing one side of a broken scale; the imbalance always remains.
Why Integrated Treatment Is the Gold Standard
For years, people dealing with both bipolar disorder and substance abuse were stuck in a frustrating, inefficient cycle. They'd go to a mental health clinic to get their mood swings under control, but that clinic couldn't help with the addiction. Then, they'd check into a rehab center that was great for sobriety but had no idea how to manage the complexities of bipolar disorder.
This disconnected approach was like trying to fix two gears that are locked together by only working on one at a time. It just doesn't work. The reality is that bipolar disorder and addiction fuel each other. You can't truly heal from one without addressing the other, which is why a unified strategy is the only path to lasting recovery.

What Does Integrated Care Actually Look Like?
Integrated treatment isn't just a buzzword; it's a fundamental shift in how we care for people with a dual diagnosis. It means one team—psychiatrists, addiction counselors, and therapists—all work together under one roof, developing a single, cohesive treatment plan. No more conflicting advice from separate doctors or crucial information falling through the cracks.
This unified model weaves together all the necessary services into a seamless recovery experience, including:
- Psychiatric Services: Getting an accurate diagnosis and the right medication to manage bipolar symptoms.
- Addiction Counseling: Digging into the behaviors, triggers, and root causes of substance use.
- Individual and Group Therapy: Building practical coping skills that apply to both conditions.
- Medication Management: Using medications to stabilize mood and also to reduce substance cravings.
"An integrated approach focuses on the whole person, addressing the unique ways bipolar disorder and substance use disorder interact in the individual. The patient learns of the relationship between the two conditions, including the importance of treating one to support recovery from the other."
Put simply, this approach ensures that progress in managing mood isn't undone by substance use, and sobriety isn't derailed by an unmanaged manic or depressive episode.
Why Integration Leads to Better Outcomes
The evidence is clear: treating substance use and bipolar disorder at the same time is far more effective than tackling them one after the other. The numbers paint a stark picture of how connected these conditions are. Research shows that the lifetime prevalence of a substance use disorder in people with bipolar disorder can be as high as 59%, with alcohol and cannabis leading the pack.
A unified treatment plan is designed to break the vicious cycle where one condition triggers the other. For example, a therapist can help someone see how a depressive episode consistently leads to drinking. At the same time, a psychiatrist can fine-tune their medication to better manage those depressive dips, removing the initial urge to self-medicate in the first place.
This table highlights the key differences between the old, fragmented model and the modern, integrated approach we use today.
Comparing Treatment Approaches For Dual Diagnosis
| Feature | Separate Treatment (Old Model) | Integrated Treatment (Modern Model) |
|---|---|---|
| Team Structure | Two separate teams (mental health and addiction) who rarely communicate. | One cohesive team of cross-trained professionals working together. |
| Treatment Plan | Two different plans, often with conflicting goals or advice. | A single, unified plan that addresses both conditions simultaneously. |
| Philosophy | "Get sober first, then we'll address your mental health." | "Let's treat the whole person at once for sustainable recovery." |
| Patient Experience | Confusing and frustrating; feels like being bounced between systems. | Coordinated and supportive; all care is available in one place. |
| Outcomes | Higher rates of relapse and dropout due to unaddressed symptoms. | Improved stability, lower relapse rates, and better long-term success. |
By building a toolkit of healthy coping mechanisms that work for both mental health and sobriety, individuals are far less likely to relapse. This often includes Medication-Assisted Treatment (MAT) as a critical component. If you're curious about how that works, you can explore the value of MAT for a dual diagnosis in our detailed guide.
Ultimately, integrated treatment provides the consistent, comprehensive support needed to find real stability. It’s considered the gold standard because it respects the complex reality of a dual diagnosis and offers a sustainable path forward for people and their families across Massachusetts.
Navigating a Dual Diagnosis Program in Massachusetts
Thinking about getting help for both substance use and bipolar disorder can feel like a lot to take on. It’s a huge first step. But knowing what to expect can turn that uncertainty into confidence. In Massachusetts, the best dual diagnosis programs lay out a clear, structured path that takes you from your first conversation all the way to building a new life in recovery.
You’re not in this alone.
The whole journey starts with a simple, confidential assessment. This isn’t an interrogation; it’s a conversation where our clinical team gets to know you as a person, not just a list of symptoms. This first meeting is absolutely essential because it lets us design a care plan that truly gets to the heart of how your bipolar disorder and substance use are connected.
Understanding Your Treatment Options
Not all treatment programs look the same—and they shouldn't. Your needs are unique, so you’ll be guided to a level of care that provides just the right amount of support without being overwhelming.
In Massachusetts, you'll often see two main outpatient structures:
- Partial Hospitalization Program (PHP): Think of this as the most intensive form of outpatient care. You’ll typically come in five days a week for several hours each day. It offers a highly structured environment with daily therapy and medical support, making it a great step down from an inpatient stay or a powerful way to prevent one.
- Intensive Outpatient Program (IOP): This option offers more flexibility. An IOP usually involves meeting three to five days a week for a few hours at a time. This setup allows you to keep up with work, school, or family life while still getting the consistent, professional support you need for both your mental health and your sobriety.
Both PHP and IOP are powerful tools for managing the complexities of substance use and bipolar disorder at the same time.
Core Therapies for Dual Diagnosis
Real, effective treatment isn’t just about talking; it’s about learning practical skills to manage mood swings and cravings at the same time. Two of the most effective and proven therapies for dual diagnosis are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
CBT helps you pinpoint and challenge the negative thought cycles that feed both depression and the urge to use. For instance, you’ll learn how to catch the thought, "I need a drink to handle this," and actively reframe it into a healthier, more productive action.
DBT is all about building real-world skills in four key areas: mindfulness, tolerating distress, regulating emotions, and building healthier relationships. It gives you a toolbox of concrete strategies to handle intense feelings without turning to substances—a game-changer when dealing with the emotional highs and lows of bipolar disorder.
By weaving these therapies together, an integrated program helps you do more than just survive a crisis. It gives you the tools to break the cycle of self-medication for good and build the emotional strength needed for lasting recovery.
The goal is to move toward a stable, fulfilling life you can be proud of.
Building Your Aftercare and Support Plan
Finishing a treatment program is a huge accomplishment, but it's important to see it for what it is: the start of a lifelong recovery journey, not the finish line. When you're managing both a substance use disorder and bipolar disorder, true, lasting recovery is built on a solid foundation of ongoing support. The best way to protect all the hard work you've put in is by creating a detailed aftercare plan.

Think of this plan as your personal roadmap for life after treatment. It's designed to help you navigate the challenges that will absolutely come up once you leave a structured program. This is all about being proactive, not just reacting when things get tough.
Crafting a Robust Relapse Prevention Strategy
A solid relapse prevention strategy is the heart of any good aftercare plan. This process begins with getting brutally honest about your personal triggers—the specific things that can set off a bipolar mood episode or a craving to use. Triggers aren't just people, places, or things; they can be internal feelings like stress, exhaustion, or loneliness.
Once you’ve identified your triggers, you can map out healthy ways to cope with them. Your plan should outline specific, constructive actions to take instead of turning to substances.
- Mindfulness and Grounding: Simple practices like deep breathing or the 5-4-3-2-1 grounding technique can be incredibly powerful for calming racing thoughts and pulling you back into the present moment.
- Physical Activity: You don't have to become a marathon runner. Even a simple walk around a park in your Massachusetts town can act as a powerful mood stabilizer and stress reliever.
- Creative Outlets: Hobbies like writing, painting, or playing music give you a healthy way to channel and express difficult emotions that might otherwise feel overwhelming.
- Structured Routine: For managing bipolar disorder, stability is key. A consistent schedule for sleep, meals, and daily tasks creates a predictable rhythm that can make all the difference.
An effective relapse prevention plan isn’t about trying to avoid all of life's stress; it’s about having a pre-planned toolkit of healthy responses ready to go when that stress inevitably shows up.
The Critical Role of Continued Support
Recovery is not a solo mission. Building a strong, reliable support network isn't just a good idea—it's non-negotiable for long-term success. The best networks include a mix of professional guidance and connections with peers who get it.
Continuing with individual therapy gives you a safe, confidential space to work through challenges and fine-tune your coping skills. For many people in Massachusetts, local peer support groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or the Depression and Bipolar Support Alliance (DBSA Massachusetts) are lifelines. These groups connect you with people who truly understand what you're going through, which is a powerful antidote to the isolation that often comes with recovery.
Involving Family and Loved Ones
Your family can be your biggest ally in recovery, but they often need guidance on how to help effectively. Family education is a crucial piece of aftercare. It teaches loved ones how to provide meaningful support without accidentally enabling old, destructive behaviors.
This process helps them understand the complexities of substance use and bipolar disorder, set healthy boundaries for themselves, and become active partners in your wellness journey. Open communication and clear boundaries can transform a home environment from one of friction into one that fosters healing for everyone.
Ready to Find Your Path Forward?
If you feel trapped in the cycle of bipolar disorder and substance abuse, please know you’re not alone, and you don’t have to walk this path by yourself. At South Shore Recovery Center, we specialize in providing the integrated, compassionate care that truly makes a difference.
Our programs are built from the ground up to treat both conditions at the same time, because we know from experience that’s what works. We offer dedicated Partial Hospitalization (PHP) and Intensive Outpatient (IOP) services right here in Massachusetts, using proven, evidence-based therapies to help you build a solid foundation for a future you can count on.
Your Journey Starts with a Single Step
We firmly believe that getting high-quality care shouldn’t be a financial burden. That’s why we work with a wide range of insurance providers to make treatment as accessible and manageable as possible. We know that reaching out is often the hardest part, and our team is here to make that first step feel safe and supportive.
Taking that first step to ask for help is an incredible act of strength. Our entire purpose is to offer a safe, confidential space where you can finally start to heal and reclaim your life from the dual grip of addiction and bipolar disorder.
Everyone’s journey toward a stable, sober life looks different. We’re committed to giving you the personalized support and clinical expertise you need to not just get well, but to thrive.
There’s no reason to wait another day. Contact our team today for a confidential chat about how we can help you or someone you care about.
Frequently Asked Questions
Why do so many people with bipolar disorder also have a substance abuse problem?
It often begins as a way to self-medicate. Individuals may use substances to dampen the high energy of a manic episode or to lift themselves out of a severe depression. This coping strategy can quickly evolve into a cycle of dependency, making both conditions more difficult to manage.
Can substance abuse cause bipolar disorder?
Substance use does not directly cause bipolar disorder. However, for someone with a genetic predisposition to the condition, heavy substance use can trigger the first manic or depressive episode and worsen the course of the illness over time.
What is "integrated treatment" and why is it important in Massachusetts?
Integrated treatment means addressing both bipolar disorder and substance abuse at the same time, with one cohesive clinical team. This approach is critical because the two conditions are deeply intertwined. In Massachusetts, leading treatment centers offer this model to prevent the "revolving door" of separate treatments, leading to better long-term outcomes, lower relapse rates, and more sustainable recovery.
What kind of support is available in Massachusetts after finishing a program?
A strong aftercare plan is key. This includes ongoing individual therapy, psychiatric medication management, and peer support. Massachusetts has numerous peer-led groups, such as local chapters of Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and the Depression and Bipolar Support Alliance (DBSA Massachusetts), which provide an essential community for long-term wellness.
How can I help a family member with a dual diagnosis?
Support starts with education and setting healthy boundaries. Encourage your loved one to seek a professional dual diagnosis assessment. Offer emotional support without enabling their substance use. Participate in family therapy sessions offered by treatment programs in Massachusetts to learn effective communication and how to be a constructive part of their recovery journey.


