Watching a family member struggle with substance use is a painful and confusing experience. It's hard to know what to say or do, and the fear of making things worse can be paralyzing. This guide is designed to give you a clear, compassionate roadmap. You'll learn how to offer effective support without sacrificing your own well-being, with specific resources available here in Massachusetts.
Key Takeaways
1. Education is Your First Step: Understand that addiction is a brain disease, not a moral failing. This knowledge is the foundation for a compassionate, effective approach.
2. Plan Your Conversation Carefully: Avoid spontaneous, emotional confrontations. A planned, calm conversation that uses "I feel" statements is far more likely to open the door to change.
3. Set Boundaries to Stop Enabling: There's a critical difference between helping and enabling. Loving boundaries—like not providing money but offering to drive them to treatment—are essential for both your well-being and their recovery.
4. Prioritize Your Own Self-Care: You cannot be a source of strength if you are depleted. Connecting with support groups like Al-Anon in Massachusetts and seeking therapy for yourself is a necessary strategy, not a selfish act.
Your First Steps in a Difficult Journey
That moment of realization—when you see that a family member has a substance use disorder—can be completely overwhelming. It’s natural to feel helpless and lost.
The most important first move is to reframe how you see the problem. Addiction is a complex brain disease, not a moral failing or a simple lack of willpower. Once you can approach the situation from that perspective, judgment starts to fade and empathy can take its place. That shift is absolutely essential for making any real progress.

This journey is a marathon, not a sprint. It requires strength, endless patience, and a clear strategy. Instead of just reacting out of fear or frustration, you can learn to respond with purpose. Let's break down those four key pillars that will form the bedrock of your approach.
The Four Pillars of Supporting a Loved One Through Addiction
To make this manageable, I've broken down the core principles into a simple framework. Think of these four pillars as your guideposts for providing effective and healthy support.
| Pillar | What It Means | Why It's Critical |
|---|---|---|
| Education | Learning about the science of addiction—how it affects the brain and behavior. | It replaces judgment with understanding and helps you respond with empathy, not anger. |
| Conversation | Planning a calm, non-confrontational talk to express your concern and offer help. | An ambush rarely works. A thoughtful conversation opens the door for them to accept help. |
| Boundaries | Defining what you will and will not do to help, protecting them from consequences. | This stops enabling behavior and protects your own well-being from the chaos of addiction. |
| Self-Care | Actively taking care of your own mental and emotional health through the process. | You cannot be a source of strength for someone else if you are completely depleted. |
Internalizing these four points will keep you grounded and focused, even when things get tough.
Pillar 1: Educate Yourself on Addiction
Before you can offer real help, you need to understand what you're up against. Taking the time to learn about the psychological and physiological roots of addiction is a game-changer.
- It’s a Disease, Not a Choice: Addiction fundamentally rewires brain chemistry. It hijacks the parts of the brain responsible for decision-making, impulse control, and judgment. This is why someone might continue using even when their life is falling apart around them.
- Co-Occurring Conditions are Common: It’s incredibly common for people struggling with addiction to also have an underlying mental health condition like depression, trauma, or anxiety. Here in Massachusetts, any effective treatment plan must address these dual-diagnosis issues together.
Pillar 2: Plan a Supportive Conversation
How you first bring up your concerns can make all the difference. An emotional, off-the-cuff confrontation almost never works and usually just pushes them further away.
The better approach is to plan a calm, private conversation. The goal isn't to win an argument or force a confession; it's simply to open a door for them to talk.
The objective is to express love and concern, not to issue ultimatums or assign blame. Frame your statements using "I" language, such as "I am worried about you," which feels less accusatory than "You have a problem."
Pillar 3: Set Loving Boundaries
There's a fine line between supporting someone and enabling their addiction. Enabling means shielding your loved one from the natural consequences of their substance use—like paying their overdue rent, making excuses to their boss, or bailing them out of trouble.
Setting firm, clear boundaries is one of the most loving and effective things you can do. For example, you might say, “I love you and I will drive you to a treatment center in Massachusetts anytime, day or night. But I can no longer give you money.”
Pillar 4: Prioritize Your Own Well-Being
You can't pour from an empty cup. The emotional toll of loving someone with an addiction is immense, and it can drain you completely if you’re not careful.
It is absolutely crucial to protect your own mental and physical health. Seeking support for yourself through therapy or groups like Al-Anon isn't selfish—it’s a necessary strategy. It ensures you have the strength to provide sustainable, healthy support over the long term.
Recognizing the Signs and Starting a Hard Conversation
It’s one of the hardest things to watch: seeing someone you love change in ways you don’t understand. Addiction can be incredibly subtle at first. It often hides behind excuses and small behavioral shifts that are easy to brush off on their own. But when you start connecting the dots, a troubling picture can emerge. The first real step toward helping your family member is learning to see past the denial and recognize the signs for what they are.
The signals of a substance use disorder aren't always what you see in the movies. It often starts quietly. You might notice them pulling away from family events they used to love, or maybe they’ve become cagey about their finances. It’s a pattern of small changes that, when pieced together, point to a much larger problem.
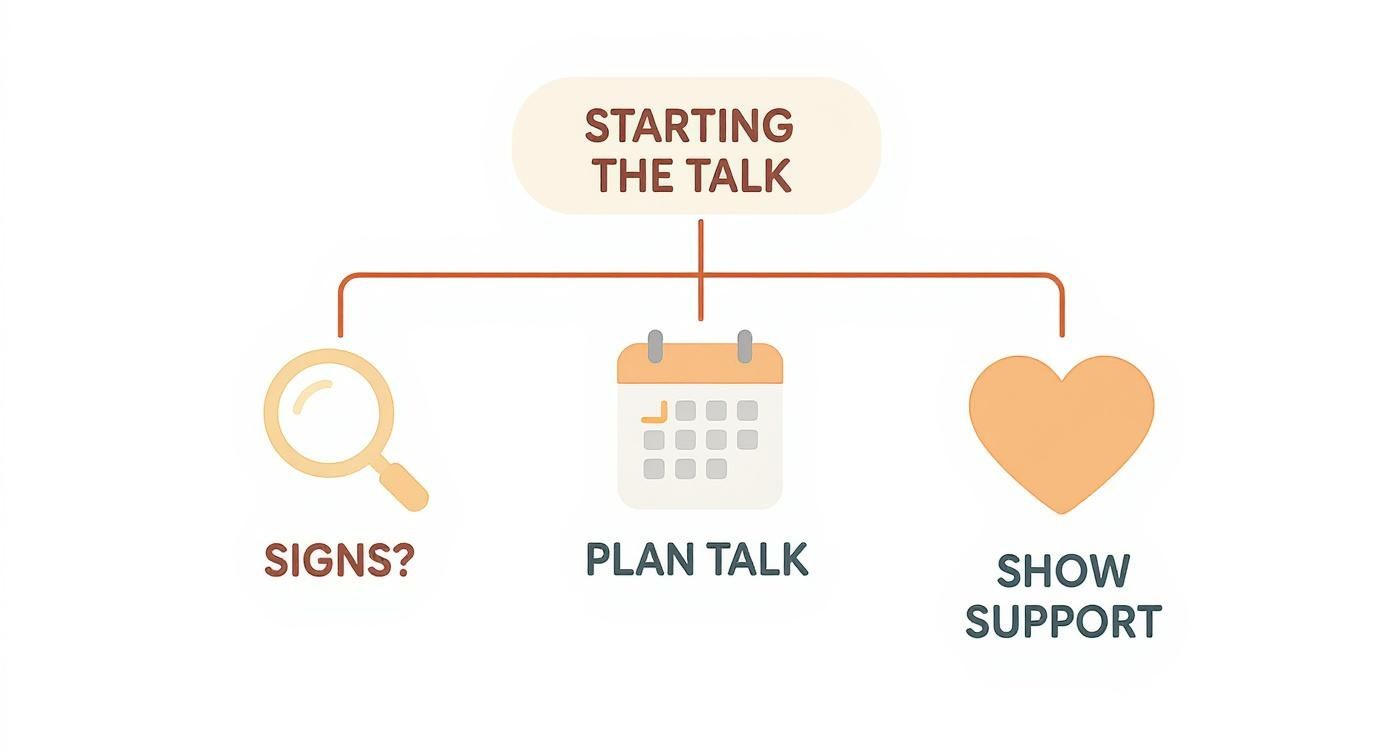
How to Prepare for This Talk
Know What You're Looking For: Knowledge is your best ally right now. When you can identify the specific behavioral, physical, and psychological indicators, you can approach the situation with clarity and facts, not just gut feelings.
Plan a Supportive, Private Moment: The how and where of this conversation are just as critical as the what. Find a time and place where your loved one will feel safe and respected, not ambushed or put on the spot.
Use "I Feel" Statements: This is crucial. Frame your concerns around your own feelings and observations. A simple "I'm worried about you" will always land better than an accusatory "You have a problem."
Brace for Any Reaction: They might respond with anger, denial, or shame. These are all common, knee-jerk reactions. Mentally prepare for this, and remember your goal isn't to force a confession on the spot, but to open a door to the possibility of change.
Identifying the Subtle Warning Signs
Before you can have "the talk," you have to be sure there’s something to talk about. While every person’s struggle is unique, some patterns are incredibly common. These signs often fall into three main buckets: physical, behavioral, and psychological.
On a physical level, you might notice things like sudden weight loss or gain, a decline in personal hygiene, or pupils that seem consistently smaller or larger than normal. Behaviorally, the signs can be even clearer. Are they dropping the ball at work or school? Are they suddenly having money troubles, borrowing or even stealing? Have old friendships faded away?
The psychological shifts can be just as telling. Look for uncharacteristic mood swings, a short temper, paranoia, or a general lack of motivation for things they used to care about. While any of these signs alone might not mean much, a consistent pattern is a serious red flag.
How to Initiate a Difficult Conversation
Once you've seen the pattern, the next hurdle is figuring out how to bring it up. This conversation is delicate, and it can set the tone for everything that comes next. If you go in guns blazing, filled with emotion and accusations, it will almost certainly backfire and could push them even further away.
Your goal here is to build a bridge, not a wall. You want to create an opening for them to accept help, and that requires a calm, supportive, and non-judgmental approach.
- Pick Your Moment Carefully: Find a private, quiet space where you won't be interrupted. Make sure neither of you is hungry, angry, lonely, or tired (HALT). And never, ever have this talk when they are under the influence.
- Decide Who Should Be There: Sometimes, a one-on-one talk is the most effective. Other times, having another trusted, calm family member there can reinforce the message of support. Just be careful not to create a situation that feels like an intervention or an ambush.
- Have a Loose Script: You don't need to read from a piece of paper, but it helps to jot down your main points beforehand. This keeps you focused if emotions run high. Center your script on your love and concern, and stick to specific, non-judgmental examples (e.g., "I was so scared when I couldn't get ahold of you last weekend and I'm worried something might have happened.").
Using Language That Heals, Not Hurts
The words you choose will make or break this conversation. You need to express your concern in a way that can actually be heard without triggering their defenses. This is where "I" statements become your most powerful tool.
Instead of saying, "Your drinking is out of control," you could try, "I feel so worried when I see how much you're drinking because I love you and I'm scared for your health." See the difference? That simple shift takes the blame out of the equation and grounds the conversation in your feelings.
Be ready for a negative reaction. Denial is a powerful part of addiction. They might get angry, minimize the issue, or even try to turn things around on you. Your job is not to win an argument. It’s to lovingly state your concern, offer your unconditional support, and plant the seed that help is available. Reassure them that you are on their team and want to help them find a way forward, whether that’s exploring treatment centers in Massachusetts or just making a call to a professional.
Figuring Out Addiction Treatment in Massachusetts
When your loved one finally agrees to get help, you might feel a huge sense of relief—quickly followed by a wave of confusion. The world of addiction treatment is a maze of acronyms and different levels of care that can feel completely overwhelming. Getting a handle on these options, especially here in Massachusetts, is the key to turning that moment of willingness into a real, effective plan for recovery.
Making sense of the treatment landscape is your first big step. From medically supervised detox to flexible outpatient programs, each level of care is designed for a specific purpose and stage of the recovery journey. When you understand the differences, you can ask the right questions and advocate for the care your family member truly needs.
The journey to treatment often starts with a difficult but necessary conversation.
As you can see, the path forward starts with recognizing the signs and planning a supportive talk. That conversation is the gateway to exploring the right treatment options together.
The Different Levels of Care: What You'll Find in MA
In Massachusetts, addiction treatment isn't a one-size-fits-all deal. It's structured as a "continuum," which just means people can move to more or less intensive programs based on what they need at any given time.
Here are the most common levels you'll come across:
- Detox (Medical Detoxification): This is usually the first stop for anyone physically dependent on substances like alcohol, opioids, or benzodiazepines. It provides 24/7 medical supervision to help them manage withdrawal symptoms safely, which can be dangerous to do alone.
- Residential or Inpatient: This means living at a treatment facility for a set period, often 30 to 90 days. It creates a highly structured, trigger-free environment where the sole focus is on healing with constant therapeutic support.
- Partial Hospitalization Program (PHP): You'll also hear this called a Day Treatment Program (DTP). It’s the most intense form of outpatient care. Clients attend programming for several hours a day, five days a week, but get to go home at night.
- Intensive Outpatient Program (IOP): An IOP is a step down in intensity from a PHP, involving fewer hours of therapy each week. It offers a solid support system while giving people the flexibility to keep up with work, school, or family life. You can learn more about how an Intensive Outpatient Program balances structure and real-world responsibilities.
- Standard Outpatient (OP): This is the least intensive level, usually consisting of one or two therapy sessions a week, either one-on-one or in a group. It's great for long-term maintenance or for those with a strong support system at home.
The right fit depends on things like how severe the substance use is, whether they're also struggling with mental health issues, and how stable their home environment is.
To help you visualize how these programs differ, here's a quick comparison.
Comparing Addiction Treatment Levels of Care in MA
This table gives a simple overview of the most common treatment programs available to families in Massachusetts, helping you understand where your loved one might best fit.
| Level of Care | Intensity and Setting | Best Suited For | Example Services |
|---|---|---|---|
| Detox | 24/7 medical supervision in a clinical setting. | Individuals at risk of severe or dangerous withdrawal symptoms. | Medical monitoring, medication management, stabilization. |
| Residential | Live-in facility with a highly structured daily schedule. | Those needing a complete break from their environment and intensive support. | Individual/group therapy, recreational therapy, holistic care. |
| PHP / DTP | 5-6 hours/day, 5 days/week at a facility; return home at night. | Individuals who need daily structure but have a stable home environment. | Structured group therapy, skills-building, case management. |
| IOP | 3-4 hours/day, 3-5 days/week at a facility; return home at night. | People transitioning from a higher level of care or who need support while working. | Group therapy, individual counseling, family sessions. |
| Outpatient | 1-2 sessions per week, often in the evenings. | Individuals maintaining long-term recovery or with mild substance use issues. | Weekly therapy sessions, support group meetings. |
Ultimately, a clinical assessment will determine the official recommendation, but having this knowledge helps you participate in the conversation.
The Therapeutic Approaches That Actually Work
It’s not just about where you go for treatment; it’s about what happens there. The best treatment centers in Massachusetts use evidence-based therapies—methods that have been proven through research to help people get better.
The most successful recovery plans don't just stop the substance use; they treat the whole person. This means getting to the root of the problem, whether it's underlying trauma, anxiety, or depression that's been driving the addiction.
You’ll hear a lot of terms, but two of the most important are:
- Cognitive Behavioral Therapy (CBT): This is a practical, hands-on approach. It helps people identify the negative thoughts and behaviors that fuel their addiction and teaches them new, healthier ways to cope with life's challenges.
- Medication-Assisted Treatment (MAT): For opioid and alcohol addiction, MAT is a game-changer. It combines behavioral therapy with specific medications (like buprenorphine or naltrexone) that reduce cravings and withdrawal symptoms. This gives the brain a chance to heal so the person can actually focus on their therapy.
How to Support Without Enabling
When you love someone struggling with addiction, your instincts tell you to help, to fix, to protect. But this is where things get tricky. There's a fine but critical line between genuinely supporting the person you love and unintentionally fueling the disease you hate.
Learning this difference is one of the most powerful and loving things you can do.
Enabling often comes from a good place—fear, love, a desperate need to keep things from falling apart. It looks like paying their rent when they can't, calling them out sick from work, or bailing them out of trouble. These actions might feel like a lifeline in the moment, but they actually soften the landing. They shield the person from the very consequences that could be the catalyst for them to finally seek help.

Real support empowers recovery, it doesn't cushion the fall from addiction. This requires a major shift in thinking, moving from short-term fixes to a long-term strategy centered on firm, clear, and consistent boundaries.
Defining Your Boundaries
Let's be clear: boundaries are not punishments. They aren’t threats or ultimatums. They are simply the rules of engagement that protect your own well-being and make it clear what you will and will not do. The focus is on your actions, not on controlling theirs.
For instance, a boundary isn't, "You have to stop using." Instead, a healthy, supportive boundary sounds like this: "I cannot have drugs in my home. If you are using, you can't stay here, but I will drive you to a treatment center in Massachusetts the second you are ready to go."
Here are a few practical examples of what this looks like in real life:
- Financial Lines: "I love you and I'm worried about you, which is why I can no longer give you money or pay your bills."
- Behavioral Rules: "We'd love for you to join us for family dinner, but if you're intoxicated, we will have to ask you to leave."
- Emotional Honesty: "I will not lie to your boss or make excuses for you anymore. It's not helping either of us."
- Logistical Help: "I am more than willing to sit with you and research treatment options or take you to an AA or NA meeting."
When you communicate these boundaries, do it with love, but also with firmness. You should expect pushback—maybe even anger. But staying consistent is absolutely crucial for both of you.
The Importance of Self-Care
Trying to support someone with an addiction is an emotionally draining marathon, not a sprint. The constant worry, the chaos, and the stress can easily lead to burnout, anxiety, and deep-seated frustration.
This is why prioritizing your own well-being isn't selfish; it's essential.
You cannot pour from an empty cup. If you neglect your own health, you will eventually have nothing left to give. Protecting your mental health allows you to show up for your loved one with the strength and clarity this journey requires.
Taking care of yourself means building your own support system. You are not alone in this.
- Al-Anon and Nar-Anon: These are incredible, free support groups designed specifically for families and friends who are navigating a loved one's addiction. You can find local meetings all over Massachusetts where you'll be in a room with people who just get it.
- Professional Therapy: A good therapist can be a game-changer. They can equip you with coping strategies, help you process the grief and anger you're feeling, and guide you in holding those tough boundaries.
- The Basics: Don't forget the fundamentals. Make sure you're sleeping enough, eating well, and moving your body. These simple acts are powerful tools for managing stress.
By taking these steps, you’re not just helping yourself. You’re modeling healthy behavior and building the resilience you'll need for the long road ahead. You show your loved one that while you can’t control their choices, you are in control of your own life and will not be pulled under by the disease. That strength can become an anchor for them when they’re finally ready to heal.
The Family’s Role in Long-Term Recovery
Getting your loved one into treatment is a huge, critical first step. But it's just that—the first step. Recovery isn’t a quick fix; it's a long road, and your family's role will shift from crisis intervention to providing a stable, supportive foundation for the journey ahead. This is where the real work of healing together truly starts.
Your active involvement can make all the difference in your loved one’s long-term success. Addiction doesn't just affect one person; it sends shockwaves through the entire family, fraying relationships and shattering communication. To heal, everyone has to learn new, healthier ways to relate to and support one another.

It’s about patiently rebuilding trust, setting realistic expectations for the future, and creating a home environment where sobriety can genuinely take root and grow.
Healing Together Through Family Therapy
Once the substance use stops, the emotional wreckage often remains. Resentment, deep-seated mistrust, and years of broken communication don’t just vanish overnight. That’s why professional family therapy is one of the most powerful tools you can have for building a lasting recovery.
In a safe, facilitated space, a therapist can help your family tackle these painful dynamics head-on. You'll learn how to express your feelings without assigning blame, set healthy boundaries with respect, and start functioning like a team again. These sessions are absolutely vital for rebuilding the trust that addiction stole from you. You can learn more about how a structured approach to family therapy for substance abuse can guide your family's healing process.
Changing Your Perspective on Relapse
For most families, the fear of relapse is a constant, nagging anxiety. It's incredibly important to understand that relapse is not a moral failure or a sign that your loved one doesn't care. For many, it's a very real part of the recovery process. Thinking of it this way helps strip away the shame and allows for a more effective response.
If a relapse does happen, the goal is to react with compassion, not anger. The immediate focus should be on getting them back into a supportive setting, figuring out what triggered the slip, and making adjustments to their recovery plan. A calm, supportive reaction from you can be the difference between a temporary setback and a full-blown return to active use.
Creating a Recovery-Friendly Home
Your home environment plays a massive role in supporting sobriety long-term. And this means more than just clearing out the liquor cabinet. It's about consciously building a culture of health, open communication, and positive reinforcement.
What does this actually look like?
- Celebrate the Wins: Make a point to acknowledge the milestones, big and small. Whether it's 30 days sober or just a stressful day handled well, recognition matters.
- Discover New Activities: Find healthy things you can enjoy together. Go hiking on the South Shore, start a weekly game night, or pick up a new hobby as a family.
- Keep the Dialogue Open: Foster an environment where your loved one feels safe enough to talk about cravings, fears, or struggles without fearing judgment.
The challenge of helping a family member is massive, especially when you consider how hard it is to get care. In 2021, an estimated 46.3 million people in the U.S. had a substance use disorder, but a staggering 6.3% actually received any treatment. These numbers highlight just how critical family support is in navigating a complex system and encouraging someone to stay engaged with their recovery.
Your steady, loving support is the most powerful tool your loved one has.
How to Get Help Today in Massachusetts
Knowing something has to change is the first step. Making that first call is the next, and it's often the hardest part. It can feel overwhelming, but taking action is the most powerful thing you can do to begin the healing process for your entire family.
Let’s walk through what happens next, one step at a time.
Your First Conversation
When you reach out, you’ll be speaking with an admissions specialist who understands what you're going through. You'll be met with compassion, not judgment. Our team at South Shore Recovery Center is here to listen, answer your questions, and give you immediate, practical advice on how to help a family member with addiction.
This first conversation is completely confidential and comes with no strings attached. We can help you verify your insurance benefits right away, so you have a clear picture of what your plan covers. Getting the financial questions answered upfront can lift a huge weight off your shoulders.
That first call is simply a conversation. It's confidential and there's no pressure. Our only goal is to give you clarity and a sense of direction, so you can move forward with confidence.
Understanding the Path Forward
During our talk, we can go over what a personalized treatment plan looks like. A big part of what we do involves family therapy, because we know that when one person is struggling, the whole family feels it. Healing together is crucial for lasting recovery.
We'll explain how our programs here in Massachusetts are set up to provide intensive support while still allowing your loved one to maintain connections to their job, school, and home life.
It's also important to know you're not alone in this. In 2023, the U.S. government allocated USD 21.8 billion to expand access to addiction treatment, showing a real national commitment to helping families just like yours. Tapping into community and governmental support is a key part of building a strong foundation for recovery. You can learn more about these public health efforts and see the latest drug abuse statistics.
The biggest takeaway? Taking action is the best antidote to fear. Making one phone call can turn that feeling of helplessness into a concrete plan for a better future.
Frequently Asked Questions
What if my family member refuses to get help?
This is a common and painful reality. If they refuse help, you cannot force them. The focus must shift to maintaining your boundaries and stopping any enabling behavior. The natural consequences of their addiction can become a powerful motivator for change. Your offer for help should always remain open for when they are ready.
Can you force someone into rehab in Massachusetts?
Yes, under specific circumstances. Massachusetts law includes Section 35, a civil commitment process that allows a court to order someone into treatment if their substance use poses an immediate and serious risk of harm to themselves or others. This is a significant legal step and is typically considered a last resort in life-threatening situations.
What is the difference between supporting and enabling?
Supporting empowers recovery, while enabling shields the person from the consequences of their addiction. Support looks like driving them to a therapy appointment or helping them research treatment options. Enabling looks like giving them money you know might be used for substances or lying to their employer for them.
Are there support groups for families in Massachusetts?
Absolutely. Al-Anon (for families of those with alcohol addiction) and Nar-Anon (for families of those with drug addiction) are invaluable resources. You can find local and virtual meetings across the state through the Al-Anon Family Groups website for Massachusetts. Connecting with others who understand your situation is crucial for your own well-being.

