Dealing with a substance use disorder is hard enough, but when it’s combined with a mental health condition like depression or anxiety, it can feel impossible to escape the cycle. This is the reality of a dual diagnosis. Fortunately, specialized dual diagnosis drug treatment offers a path forward by addressing both issues at the same time. This integrated approach is the key to building a strong, sustainable recovery.
Key Takeaways
- Integrated Treatment is Essential: True recovery requires treating both the substance use disorder and the mental health condition simultaneously. Addressing one without the other often leads to relapse.
- Personalized Care is Key: Effective treatment plans utilize evidence-based therapies like CBT and DBT but are tailored to the individual's specific needs, addressing their unique triggers and challenges.
- Levels of Care in Massachusetts: The state offers a continuum of care, from medically supervised detox to structured outpatient programs like Day Treatment (PHP) and Intensive Outpatient (IOP), ensuring you get the right level of support.
- Support Systems are Crucial for Success: Lasting recovery is built on a strong foundation that includes family involvement, peer support groups, and a comprehensive aftercare plan to navigate life after treatment.
The Dual Challenge of Addiction and Mental Health

When mental illness and substance use exist together, they create a vicious cycle that’s incredibly hard to escape on your own. A person might turn to alcohol to quiet their racing thoughts from anxiety, only to find the substance makes their anxiety spiral even worse in the long run. This isn't a rare situation; it’s a reality for millions of people who need specialized, understanding care.
The numbers really put this into perspective. In 2023, a staggering 20.4 million adults in the United States were dealing with both a mental health disorder and a substance use disorder. This isn't a niche problem—it's a widespread public health issue that shows just how deeply these two challenges are intertwined. You can discover more insights from the National Survey on Drug Use and Health to see the full scope.
Your Guide to Understanding Integrated Recovery
For a long time, the standard approach was to treat these conditions separately. Someone might be told, "Get sober first, and then we'll work on your depression." But how can you stay sober when the untreated depression makes just getting through the day feel impossible?
Effective dual diagnosis drug treatment breaks that dead-end cycle. It brings everything under one roof, with a single, unified team that addresses both issues simultaneously.
This guide will serve as your roadmap, helping you understand this life-saving approach, particularly for those seeking help right here in Massachusetts. We’ll walk through the core principles, therapies, and program structures that empower people to reclaim their lives.
Why Integrated Treatment Is a Game Changer
For years, the standard approach to treating addiction and mental health was like trying to fix a complex machine one gear at a time, hoping the rest would somehow fall into place. People were often told, "Get sober first, then we’ll work on your anxiety." This old-school, sequential method created a revolving door of relapse, leaving countless individuals feeling stuck and hopeless.
The problem is, substance use and mental health conditions are rarely separate issues; they are deeply intertwined. Trying to solve one without the other is like bailing water out of a boat without plugging the leak. This is where a modern, integrated treatment model truly changes the game.

From Fragmented Care to a Unified Plan
Imagine a man in Massachusetts struggling with alcohol use disorder and severe social anxiety. Under the old model, he'd see an addiction counselor who might not be trained in anxiety disorders. He'd also see a separate therapist for his anxiety, but that therapist might have little experience with the realities of addiction. The two professionals may never even speak to each other.
This fragmented approach just doesn't work. His anxiety fuels his drinking, and his drinking makes his anxiety worse. Without a team that sees the whole picture, he's left trying to manage these deeply connected problems in isolation.
Integrated dual diagnosis treatment completely flips this script. From the very first assessment, clinicians work to understand exactly how both conditions interact. This leads to a single, unified care plan where every specialist is on the same page.
How a Collaborative Team Works
In an integrated setting, therapists, psychiatrists, and addiction specialists function as one cohesive unit. It’s a collaborative approach that ensures every aspect of a person's well-being is addressed at the same time.
Here’s what that looks like in practice:
- Comprehensive Assessment: Your initial evaluation doesn't just check boxes; it maps out how your substance use and mental health condition influence one another.
- Unified Treatment Plan: Instead of two separate plans, you get one master plan. Your therapy for anxiety, for example, will directly incorporate strategies for managing cravings that pop up during social stress.
- Coordinated Care Team: The psychiatrist who might prescribe medication for depression is in constant communication with your addiction counselor to ensure the treatment is complementary and safe.
- Holistic Healing: The focus is on treating the whole person, not just a collection of symptoms. This builds a much stronger, more resilient foundation for lasting recovery.
The demand for this superior model is growing fast. The global Dual Diagnosis Treatment Facility market has seen remarkable expansion, which shows just how much people need this kind of integrated care. Between 2020 and 2025, the market grew at a compound annual rate of 12.50%, hitting a value of $6.8 billion. Projections show it soaring to $12.6 billion by 2033—a clear testament to its effectiveness. You can learn more about the growth of integrated care facilities and why they lead to better outcomes.
By addressing the root causes of addiction and stabilizing mental health at the same time, integrated treatment empowers individuals to build healthier coping skills, gain emotional stability, and dramatically reduce the risk of relapse.
Choosing a specialized dual diagnosis program in Massachusetts means giving yourself or your loved one the best possible chance at success. It’s an investment in a recovery that isn’t just about stopping substance use, but about building a healthier, more resilient life from the ground up.
Core Therapies That Power Recovery
Effective dual diagnosis treatment isn’t a single, magic-bullet solution. It’s a carefully woven fabric of proven therapeutic strategies designed to work together. These therapies are the tools that empower you to understand, challenge, and ultimately change the deeply connected patterns of substance use and mental health struggles.
Think of it like this: just treating the substance use is like mopping up a flooded floor without fixing the leaky pipe. These therapies get to the source of the problem, giving you the skills not just to get sober, but to build a life where you no longer need substances to cope.
Retraining Your Brain with Cognitive Behavioral Therapy
Cognitive Behavioral Therapy, or CBT, is a workhorse in addiction and mental health treatment for a reason. It’s built on a simple yet profound idea: it's not the events in our lives that cause our distress, but our thoughts about those events.
For someone navigating a dual diagnosis, this is a game-changer. Imagine a person with depression and an alcohol use disorder whose automatic thought is, "I messed up again, I'm a total failure." That thought fuels feelings of hopelessness, which then triggers the urge to drink. CBT gives you the power to catch that destructive thought, examine it, and reframe it into something more realistic and helpful, like, "I made a mistake, but it doesn't define me. What can I do differently next time?"
By changing the thought, you break the chain reaction that leads to substance use. You can learn more about how professionals apply Cognitive Behavioral Therapy for addiction treatment and see just how practical it is.
Building Emotional Resilience with Dialectical Behavior Therapy
While CBT is about changing your thoughts, Dialectical Behavior Therapy, or DBT, is all about learning to manage overwhelming emotions. It’s especially powerful for people who feel like they're on an emotional rollercoaster, which is a common experience in dual diagnosis.
DBT teaches practical, real-world skills across four key modules:
- Mindfulness: Learning to stay grounded in the present moment without judgment.
- Distress Tolerance: This is your "break glass in case of emergency" toolkit. It teaches you how to survive a crisis without turning to drugs or alcohol.
- Emotion Regulation: Gaining control over your emotions instead of letting them control you.
- Interpersonal Effectiveness: Learning how to ask for what you need and set boundaries in a healthy way.
For instance, someone with anxiety might feel a panic attack coming on. Instead of immediately reaching for a substance to numb the feeling, DBT provides concrete skills—like holding ice or using a specific breathing technique—to ride the wave of panic until it passes.
Finding Your Inner Drive with Motivational Interviewing
Let’s be honest: recovery only works if you want it. That’s where Motivational Interviewing, or MI, comes in. This isn't a therapist lecturing you about what you should do. It's a collaborative conversation designed to help you find your own reasons for making a change.
An MI-trained therapist acts more like a guide, asking open-ended questions to help you explore your own mixed feelings about substance use. You might discuss what you like about it, and what you don't. This respectful, non-judgmental process helps you resolve that internal conflict and tap into a powerful, personal motivation that is far more lasting than any external pressure.
At its core, dual diagnosis treatment is about equipping you with a personalized toolkit of coping strategies. It’s not just about stopping a behavior; it's about building a new way of thinking, feeling, and living.
Supporting Healing with Medication-Assisted Treatment
Therapy and medication often work best as a team. Medication-Assisted Treatment (MAT) is an evidence-based approach that combines FDA-approved medications with counseling to treat substance use disorders, especially those involving opioids and alcohol.
These medications aren't a substitute for recovery; they're a tool that supports it. They work by stabilizing brain chemistry, reducing intense cravings, and blocking the rewarding effects of substances. This provides the mental and physical stability needed to fully engage in the hard work of therapy.
The results are hard to ignore. We know that depressive disorders are incredibly common, affecting 35.5% of people with alcohol use disorder. MAT can help manage those underlying symptoms. In fact, studies show patients receiving medication for opioid use disorder were five times less likely to overdose. It's no wonder that the use of MAT for opioids grew from 12% to 31% between 2012 and 2020 as its effectiveness became clear.
Finding the Right Level of Care in Massachusetts
Making the decision to seek help for a dual diagnosis is a huge step. The next, and just as critical, is figuring out what kind of help you need. Not all treatment programs are created equal, and the right one for you hinges on a few key things: the severity of your substance use, the state of your mental health, and what your day-to-day life looks like.
Here in Massachusetts, the treatment system is set up as a "continuum of care." Think of it as a series of steps, each one designed to give you the right amount of support at the right time. You can step in at the level you need and then move to a different level of support as you get stronger in your recovery.
Medically Supervised Detox: The First Step
Before you can really dig into the emotional and psychological work of recovery, your body needs to be safely and comfortably free from substances. That's where detoxification comes in.
This is a medically supervised process where a team of professionals helps you manage withdrawal symptoms 24/7. It usually takes several days. Detox isn't just about "waiting it out"—it's an essential first step for anyone with a physical dependency. Withdrawal can be incredibly difficult and sometimes even dangerous, so having medical oversight is crucial for a safe and stable transition into the next phase of your treatment.
The infographic below shows how different therapeutic paths are chosen based on whether the primary challenge is rooted in your thoughts, emotions, or motivation.
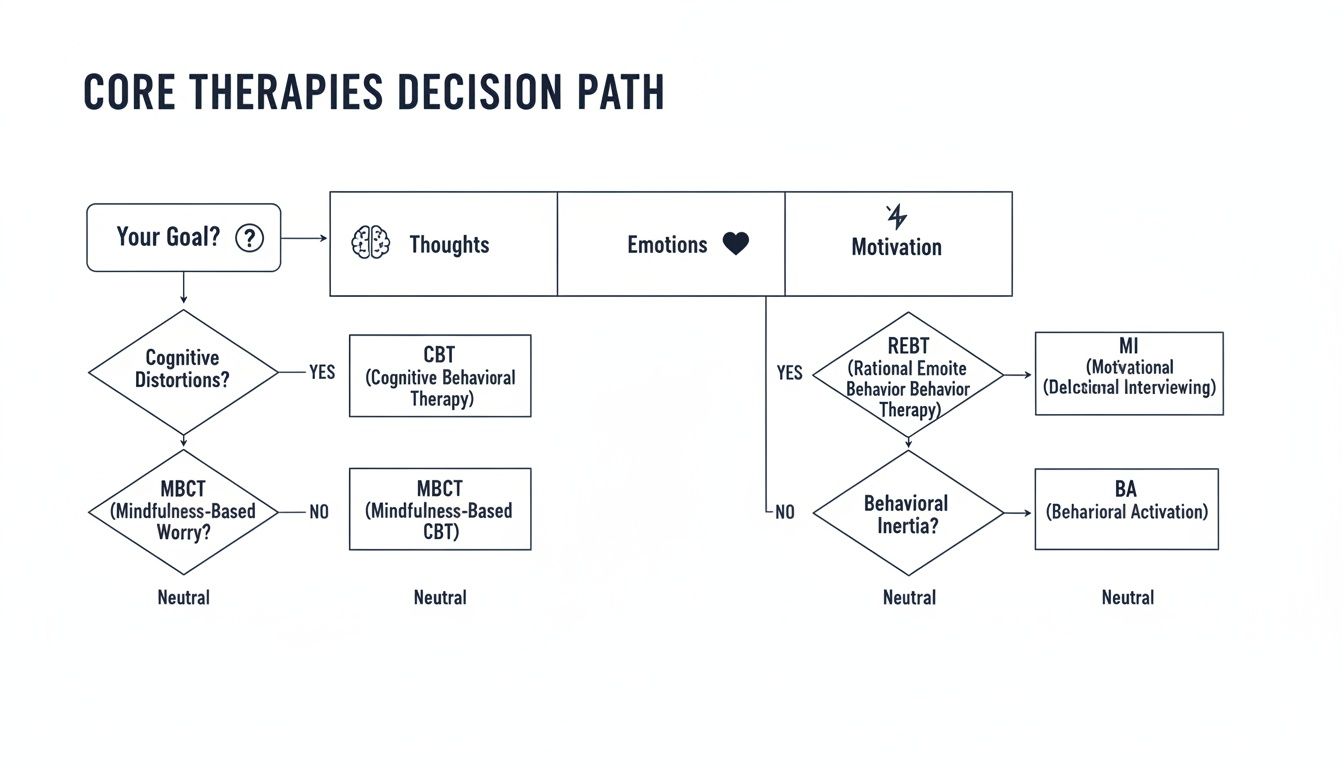
As you can see, the therapies we use aren't one-size-fits-all. They're selected to address your specific internal struggles, which is why a personalized plan makes all the difference.
Structured Outpatient Programs: Day Treatment and IOP
Once you're medically stable, the real work begins. Many people in Massachusetts find that structured outpatient programs offer the perfect balance—intensive, effective care that still allows them to live at home and manage daily responsibilities.
-
Day Treatment Programs (DTP): Often called Partial Hospitalization Programs (PHP), this is our most intensive outpatient option. You’ll join us for about five to six hours a day, five days a week, for a mix of individual therapy, group counseling, and workshops that teach you practical coping skills. It’s an ideal step for someone leaving an inpatient facility or anyone who needs significant daily support to stay on track.
-
Intensive Outpatient Programs (IOP): This is a step down from DTP but still provides a high level of structure and support. An IOP typically involves three-hour sessions, three to five days a week. This format works incredibly well for people who are gaining solid footing in their recovery but still need consistent guidance, or for those juggling treatment with a job, school, or family life.
Both our DTP and IOP are built on an integrated care model. We use proven therapies like CBT and DBT to tackle both substance use and mental health conditions together, because we know they're two sides of the same coin.
You can get a closer look at the different levels of treatment at South Shore Recovery Center and see how each one is designed to build a foundation for lasting recovery.
Finding the right fit isn't about choosing the "best" program—it's about choosing the program that's best for you right now. The right level of care provides the exact amount of support you need to build a strong foundation for a sober, healthy life.
Building Your Support System for Lasting Success
Walking out the door after finishing a dual diagnosis drug treatment program is a massive accomplishment, but it's not the end of the journey. In fact, it's the beginning of a new one. True, lasting recovery is built on a strong foundation of support that reaches far beyond the structured environment of a treatment center. It takes root when family is involved and a solid plan is in place to handle the curveballs of everyday life.
Recovery is never a solo mission. It's a process that deeply impacts, and is impacted by, the people closest to you.

Why Family Involvement is a Game Changer
When one person is grappling with a dual diagnosis, the ripple effects touch the entire family. Trust gets chipped away, communication lines get crossed, and relationships become tense. This is why involving the family isn't just a nice "extra"—it's a critical piece of the healing puzzle for everyone.
Family therapy creates a safe, guided space where loved ones can finally learn about the complex nature of co-occurring disorders. It helps everyone understand that addiction and mental illness are not character flaws but real health conditions. Just as importantly, it gives families practical tools: new ways to communicate and healthier methods for supporting their loved one without accidentally enabling harmful behaviors.
Through this process, families can start to rebuild trust and create a home environment that actively encourages sobriety—something that makes all the difference for someone returning to their community here in Massachusetts.
Crafting a Powerful Aftercare Plan
Leaving the 24/7 structure of a treatment program can feel like stepping off a cliff. It's a big, and sometimes scary, transition. A well-thought-out aftercare plan is your personal roadmap for navigating early recovery, giving you the structure and resources you need to protect your progress.
An aftercare plan isn't just a list of suggestions; it's a personalized, strategic toolkit designed to help you build a resilient, sober life one day at a time. It’s the bridge between the intensive support of treatment and the realities of long-term recovery.
A solid aftercare plan is detailed and customized just for you. It typically brings several key elements together to form a strong safety net.
- Ongoing Therapy: Sticking with individual therapy is essential for managing mental health symptoms and having a dedicated space to work through challenges as they pop up.
- Specialized Support Groups: Groups like Dual Recovery Anonymous (DRA) or SMART Recovery connect you with a community of peers who truly get the unique challenges of balancing addiction and mental health.
- Sober Living Homes: For anyone needing a bit more structure, sober living homes in Massachusetts offer a substance-free environment with built-in accountability and peer support.
- Peer Support Networks: Working with a recovery coach or a sponsor gives you invaluable guidance from someone who has been there and successfully navigated a similar path.
The best treatment programs don't just focus on getting you sober. They empower you and your loved ones with the skills, tools, and continuous support systems needed to build a genuinely fulfilling life in recovery. This kind of proactive planning is what turns a short-term win into lifelong success.
How to Find and Afford Treatment in Massachusetts
Figuring out the logistics of finding and paying for dual diagnosis drug treatment can feel like the biggest barrier to getting help. It's often overwhelming. But the good news is that high-quality, effective care is within reach right here in Massachusetts.
Once you know how to find the right facility and make sense of your insurance options, a confusing process can quickly become a clear, manageable plan.
That first step is usually just a phone call. Admissions specialists at treatment centers are pros at walking you through the entire process. They can answer your questions about the programs and, just as importantly, help you figure out the financial side. Their entire job is to make this initial stage as smooth as possible.
Demystifying Your Insurance Coverage
For most people in Massachusetts, health insurance is the primary way to cover the cost of treatment. Major providers like Blue Cross Blue Shield of Massachusetts, Tufts Health Plan, and Harvard Pilgrim Health Care are required by law to offer coverage for substance use and mental health services.
But the key is understanding what your specific plan covers. That's where an admissions team really helps.
They’ll handle a few crucial steps for you:
- Benefit Verification: They contact your insurance provider directly to confirm exactly what’s covered, including different levels of care like Day Treatment or Intensive Outpatient Programs.
- Understanding Costs: They can translate confusing insurance terms like deductible (what you pay before insurance starts paying), copay (your flat fee for a session), and coinsurance (the percentage of the cost you’re responsible for).
- In-Network vs. Out-of-Network: They'll confirm if the center is "in-network" with your insurance, which is what you want—it means you get the best coverage and pay the least out-of-pocket.
Many centers, South Shore Recovery Center included, offer a fast, confidential way to get started online. You can easily verify your insurance benefits for treatment to get a clear, no-surprises picture of your coverage.
Key Questions to Ask Any Treatment Center
When you call a potential provider, having a few questions ready empowers you to make a solid decision. This is your chance to make sure the program is truly the right fit.
Choosing a treatment center is one of the most important decisions you'll make. Ask direct questions about their approach to dual diagnosis, staff credentials, and aftercare planning to ensure you're getting comprehensive, evidence-based care.
Think about asking questions like these:
- Do you have specific programs for dual diagnosis? You want to make sure they offer truly integrated care, not just two separate tracks running side-by-side.
- What evidence-based therapies do you use? Look for names you recognize, like CBT, DBT, and MAT. This shows their methods are proven to work.
- What does a typical day or week look like? This gives you a real feel for the program's structure and intensity.
- How do you involve families in the treatment process? Family support can be a game-changer for long-term recovery, so it's a great sign when a center includes them.
Finding the right dual diagnosis drug treatment in Massachusetts is absolutely possible. By asking the right questions and getting a little expert help with your insurance, you can find the care you need to build a real foundation for recovery.
Frequently Asked Questions
What exactly is a dual diagnosis?
A dual diagnosis, also known as a co-occurring disorder, is when a person has both a substance use disorder (like an addiction to alcohol or opioids) and a mental health condition (such as depression, anxiety, PTSD, or bipolar disorder) at the same time. The conditions are interconnected and often make each other worse.
How do I know if I need dual diagnosis treatment?
If you use substances to cope with feelings of anxiety or depression, or if your mental health worsens when you try to get sober, you may have a co-occurring disorder. A professional assessment is the only way to know for sure and is the best first step toward getting the right kind of help.
What makes integrated treatment different?
Integrated treatment addresses both the substance use and mental health conditions simultaneously with a single, coordinated care team. This is different from traditional models that treat the issues separately, which can lead to fragmented care and a higher risk of relapse. An integrated approach provides a more holistic and effective path to recovery.
Can someone be forced into treatment in Massachusetts?
Yes, under a civil commitment law known as Section 35, a court can order involuntary treatment if a person's substance use poses a serious risk of harm to themselves or others. However, this is a last resort, and voluntary treatment driven by personal motivation is always the preferred and most effective path.

