When you're struggling with depression, it can feel like you're caught in a thick, heavy fog. For many, using substances seems like a way to find a brief moment of light. The most effective depression and addiction treatment tackles both of these challenges at the same time, because one condition almost always fuels the other. This integrated approach, available right here in Massachusetts, is truly the best path toward breaking that cycle for good.
Four Key Takeaways for Your Recovery Journey
Figuring out the world of treatment can feel overwhelming, but keeping these core ideas in mind will help you make clear, confident decisions for yourself or someone you care about.
- Integrated Treatment is a Non-Negotiable. You have to address both the depression and the addiction simultaneously. If you only focus on one, the untreated condition will almost certainly trigger a relapse down the road.
- You Are Not Alone. This is far more common than people realize. In fact, nearly one-third of adults with a substance use disorder also live with a co-occurring mental health condition like depression. Reaching out for specialized care is a sign of incredible strength.
- Recovery is a Process, Not a Quick Fix. Healing doesn’t happen overnight, and it's rarely a straight line. It involves a combination of proven therapies, and sometimes medication, to help you build new, healthy coping skills and find mental stability. The whole journey requires patience and a strong support system.
- Help is Available Right Here in Massachusetts. From the South Shore to the Boston area, there are many excellent outpatient programs designed specifically for co-occurring disorders. Finding the right local dual diagnosis treatment gives you the structured support you need to build a solid foundation for your recovery.
Understanding the Link Between Depression and Addiction
Depression and substance use are often tangled together in a complicated and exhausting cycle.
It’s best to think of it as a feedback loop. The constant feelings of sadness, hopelessness, and low energy that come with depression can easily lead someone to self-medicate with drugs or alcohol, just to get a moment of relief. The problem is, substance use almost always makes depressive symptoms worse in the long run, which only deepens the need for that temporary escape.
This creates a powerful downward spiral. Soon, the consequences of addiction—strained relationships, trouble at work, or financial stress—pile on, intensifying feelings of guilt and despair. This, in turn, fuels the underlying depression. Trying to treat only the addiction without getting to the root of the depression is like bailing water out of a sinking boat but ignoring the huge hole in the bottom. Real, lasting recovery requires a plan that addresses both problems at once.
The Vicious Cycle of Co-Occurring Disorders
This visual really helps show how depression and substance use feed off each other, creating a cycle that’s incredibly difficult to break out of without the right professional support.
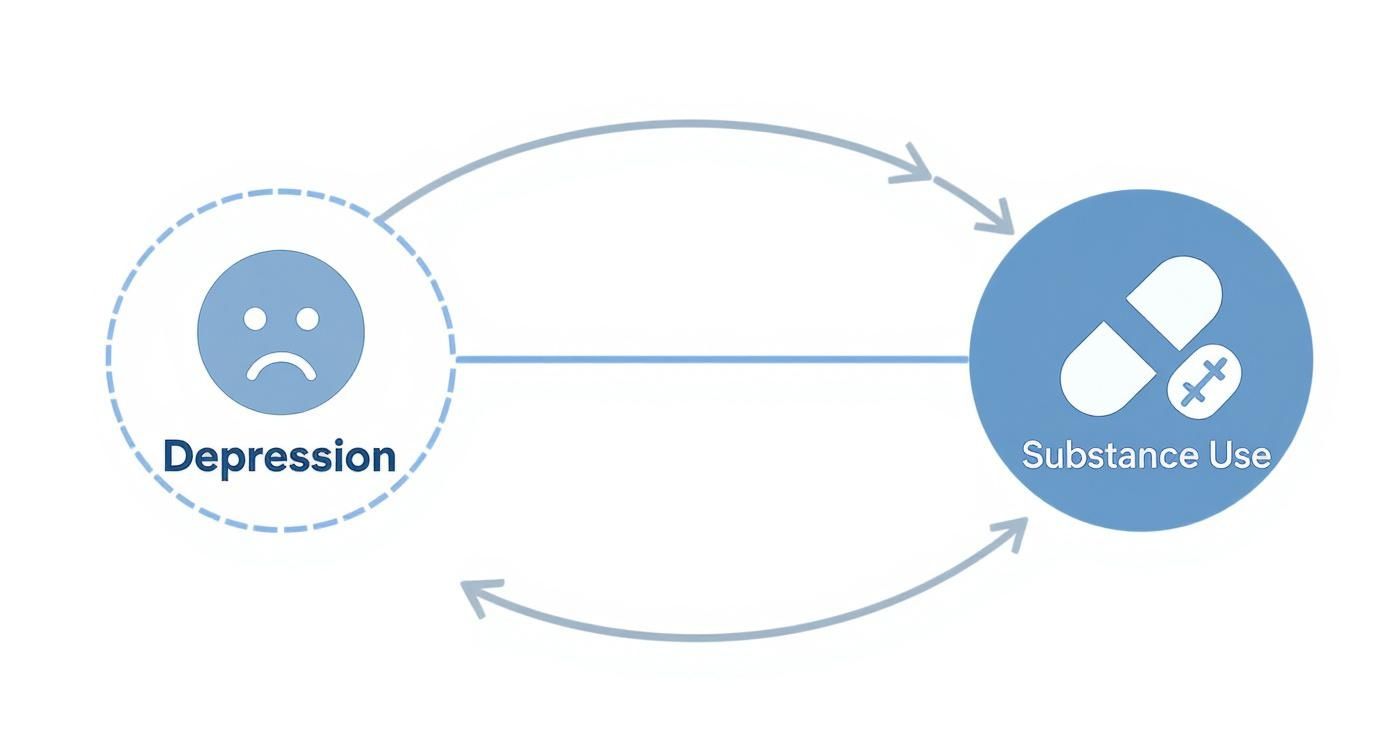
As you can see, each condition directly worsens the symptoms of the other. That’s precisely why an integrated treatment approach isn't just a good idea—it's essential.
Why Integrated Treatment Is Your Strongest Path to Recovery
When you're struggling with both depression and an addiction, it can feel like you're fighting a war on two fronts. Trying to treat them one at a time is a common mistake, and frankly, it just doesn't work.
Think of it like trying to plug two holes in a sinking boat. If you only focus on one, the water keeps pouring in through the other. You can make incredible progress with your sobriety, only to have untreated depression sneak back in and pull you right back to square one. On the flip side, it's nearly impossible to manage depressive symptoms when substance use is constantly throwing your brain chemistry and emotional stability into chaos.
The Problem with Separate Treatments
Juggling appointments at a substance use clinic and a separate mental health office creates a massive gap in your care. Your therapists aren't talking to each other, your doctors aren't on the same page, and you're stuck in the middle with conflicting advice and a treatment plan full of holes.
This disconnected approach completely misses how deeply intertwined these two conditions are. It's why a unified, integrated approach is absolutely essential for anyone who wants to find lasting wellness.
An integrated depression and addiction treatment program puts all the experts you need under one roof. In facilities across Massachusetts, from Plymouth to the surrounding South Shore communities, this model means your addiction counselors and psychiatric team are working together, collaborating on your care every single day.
This unified strategy leads to more accurate diagnoses, keeps people more engaged in their own recovery, and delivers significantly better long-term outcomes. Why? Because nothing gets missed. It builds a foundation strong enough to support you as you heal from both conditions at the same time.
How Integrated Care Works in Massachusetts
Let's make this real. Imagine you're in an outpatient program here in Massachusetts and you're suddenly hit with a crushing wave of depression. If your treatment isn't integrated, you might have to wait weeks for an outside psychiatry appointment, leaving you vulnerable.
In an integrated program, however, your addiction therapist can walk down the hall and consult with the on-site psychiatric team immediately. Your care plan can be adjusted that very same day.
This rapid, coordinated response is the superpower of integrated treatment. It gives you the right tools to manage both conditions at once, building a far more resilient foundation for your future. The reality is, without it, many people simply fall through the cracks. The numbers paint a grim picture: among adolescents with both a Major Depressive Episode and a substance use disorder, a staggering 27.9% received neither substance use treatment nor mental health care. Learn more about these important statistics on the National Depression Hotline. This gap is precisely why accessible, integrated programs are so vital.
Choosing a local program in Massachusetts that specializes in dual diagnosis means you're doing more than just stopping the use of a substance. You're getting to the root of the problem and healing the underlying issues that drive both conditions. This comprehensive care is, without a doubt, the most reliable path toward a sustainable recovery and a healthier, more fulfilling life.
Therapies That Heal Both Mind and Behavior
Getting better isn't just about wanting to change. It’s about building a completely new toolkit for handling thoughts, feelings, and actions. That’s where evidence-based therapies come in. These aren't just talk sessions; they are structured, proven methods for healing the deep-rooted issues that drive both depression and addiction. They teach you practical, real-world skills for a new way of living.
These therapies are the bedrock of good dual diagnosis care here in Massachusetts. They help you unravel the tangled wires connecting depressive thoughts to addictive urges, giving you back the control you've been missing.

Cognitive Behavioral Therapy: Rebuilding Your Thought Patterns
Cognitive Behavioral Therapy (CBT) works from a simple but profound idea: your thoughts, feelings, and behaviors are all linked. When you're struggling with depression and addiction, this link creates a vicious cycle. A thought like, "I'm worthless," can trigger a powerful craving, and giving in only deepens the despair.
CBT gives you the tools to spot those automatic negative thoughts and question them. It’s not about pretending problems don't exist. It's about learning to respond to them in a healthier way.
For instance, you might catch yourself thinking, "I messed up again, I might as well get high." CBT teaches you to press pause, identify that thought for what it is—a cognitive distortion—and reframe it: "I made a mistake, but that doesn't make me a failure. Using will only make this worse." That single moment of intervention can break the chain reaction. To dig deeper, you can explore the powerful role of CBT in addiction treatment and see how it builds lasting resilience.
Dialectical Behavior Therapy: Mastering Emotional Regulation
When your emotions feel like a tidal wave, the instinct is to find an escape. For so many people with co-occurring disorders, substances become that escape hatch. Dialectical Behavior Therapy (DBT) tackles this head-on by teaching you concrete skills to manage intense emotions without resorting to self-destructive habits.
DBT is a game-changer for anyone who feels emotionally dysregulated or experiences severe mood swings. It’s built on four core skill sets:
- Mindfulness: How to stay grounded in the present moment, observing your thoughts and feelings without getting swept away by them.
- Distress Tolerance: Practical ways to survive a crisis without making it worse.
- Emotion Regulation: How to understand your emotions and become less vulnerable to the painful ones.
- Interpersonal Effectiveness: Learning to ask for what you need and set boundaries in a way that respects yourself and others.
Think of DBT as the "owner's manual" for your emotions. It gives you a roadmap to navigate emotional storms, which is absolutely essential for both your mental health and your sobriety.
Motivational Interviewing: Finding Your Inner Drive
Real, lasting change can't be forced on someone—it has to come from the inside. Motivational Interviewing (MI) is a gentle, collaborative counseling style that helps you find your own personal reasons for wanting to change. It's the complete opposite of old-school confrontational approaches that just make people defensive.
An MI therapist partners with you to explore your mixed feelings about recovery. They won’t lecture you on why you should change. Instead, they’ll ask questions that help you see the gap between where you are and where you truly want to be.
The heart of Motivational Interviewing is making you an active partner in your own recovery. By connecting your actions to your core values and goals, it strengthens your own commitment to building a life you’re proud of.
This approach is so powerful in depression and addiction treatment because it honors your independence. It helps you find your "why," and that reason becomes the fuel that keeps you going when the journey gets tough.
To help clarify how these approaches work together, here’s a quick breakdown of their distinct roles in an integrated treatment plan.
Comparing Therapeutic Approaches for Dual Diagnosis
| Therapy | Primary Focus | Key Benefit for Dual Diagnosis |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifying and changing negative thought patterns and behaviors. | Directly breaks the cycle where depressive thinking fuels substance use. |
| Dialectical Behavior Therapy (DBT) | Building skills for emotion regulation, distress tolerance, and mindfulness. | Provides tools to manage intense emotions without turning to substances. |
| Motivational Interviewing (MI) | Exploring and strengthening internal motivation to change. | Empowers individuals by helping them find their own reasons for recovery. |
Each of these therapies offers a different piece of the puzzle. When used together in a comprehensive plan, they provide a powerful, multi-faceted approach to healing both depression and addiction from the inside out.
Finding the Right Outpatient Program in Massachusetts
Trying to find the right depression and addiction treatment can feel like an impossible task, especially when you're already feeling completely worn down. The good news is that outpatient care here in Massachusetts offers a really effective path forward—one that’s structured but flexible enough to let you get help without completely stepping away from your life.
The trick is figuring out which program matches the level of support you need at this moment.
Think of it like recovering from a serious injury. You wouldn't go from the operating table straight to running a marathon. You’d move through stages, from intensive physical therapy to less frequent check-ins. Outpatient treatment for a dual diagnosis works the same way. You find the right intensity based on your clinical needs, your lifestyle, and your responsibilities at home.
Day Treatment Programs (PHP)
The highest level of outpatient support you can get is a Day Treatment Program, which you’ll often hear called a Partial Hospitalization Program or PHP. It’s built for people who need that daily, intensive structure to stay on track but are stable enough to go home at night. It's the perfect step down from a residential facility or a necessary step up when standard therapy just isn't cutting it.
- Time Commitment: It’s a real commitment, typically running five days a week for several hours each day.
- Structure: Your days are packed with individual and group therapy, psychiatric appointments, and workshops designed to build practical coping skills.
- The Analogy: This is the intensive, daily physical therapy you’d need right after surgery. It takes a lot of your time, but it provides the rigorous support you need to get stable and start healing properly.
This highly structured format creates a strong, safe container for early recovery. It helps you build a solid foundation before you’re ready for a more independent setting.
Intensive Outpatient Programs (IOP)
An Intensive Outpatient Program (IOP) is the next step down. It strikes a great balance between serious clinical support and the flexibility to live your life. An IOP is an excellent fit if you’re feeling more stable but know you still need consistent, structured therapy to manage cravings and get to the bottom of your depression and substance use.
This is where you can keep up with work, school, or family while still getting a high level of care a few times a week. You can learn more about finding an effective outpatient addiction treatment on the South Shore of MA and see if this model makes sense for you.
An IOP is that crucial bridge between the all-in intensity of early treatment and the reality of long-term recovery. It’s where you take the skills you’ve learned and start applying them to real-world problems, building true resilience against triggers.
- Time Commitment: You’ll typically meet three to four times a week, with sessions lasting a few hours.
- Focus: The work continues to be therapeutic, with a heavy emphasis on preventing relapse and learning how to manage your emotions in a healthy way.
- The Analogy: Think of an IOP as a multi-week fitness program with a personal trainer. It’s not as all-consuming as daily physical therapy, but it gives you the consistent guidance and accountability you need to build lasting strength.
Outpatient Programs (OP)
Finally, there are standard Outpatient Programs (OP), which offer the most flexibility. This is often the last step in the treatment journey, but it can also be a starting point for someone who has a strong support system and whose symptoms are less severe. For most, OP means meeting with a therapist or counselor regularly, maybe once a week.
This level of care is all about maintenance—helping you protect the progress you've made and deal with life's curveballs as they come. It provides that ongoing touchpoint to reinforce healthy habits and catch any potential issues before they become big problems.
- Time Commitment: Usually one or two sessions per week, based on what you and your clinician decide is best.
- Purpose: This is your long-term support system, like a regular wellness check-in to make sure everything stays on track.
- The Analogy: Standard outpatient care is like having a long-term personal trainer. You've already built the muscle and know the right form; these sessions help you maintain that strength, fine-tune your approach, and stay focused on your goals.
Combining Medication with Holistic Support
Treating depression and addiction effectively isn't just about what happens in a therapist's office. Real, lasting healing requires a balanced approach that supports your mind, body, and spirit. It’s about pairing the right medical tools with holistic practices that build the resilience you need for the long haul.
Medication can be a game-changer. For someone crushed by the weight of depression and fighting the constant pull of cravings, tools like antidepressants or Medication-Assisted Treatment (MAT) can feel like a lifeline. They work on a biological level to help stabilize brain chemistry, which can dial down depressive symptoms and reduce the intense physical urge to use.
It’s helpful to think of these medications as a support system, not a magic bullet. Imagine a cast on a broken leg. The cast itself doesn't heal the bone, but it provides the stability and protection needed for the body to do its own healing work. In the same way, medication can create the mental and emotional stability necessary to dig in and get the most out of therapy.
The Role of Medication in Dual Diagnosis Care
Medication-Assisted Treatment (MAT) is an especially powerful tool when we're talking about co-occurring disorders, particularly for those involving opioid or alcohol addiction. MAT is an evidence-based approach that combines FDA-approved medications with counseling and behavioral therapies to treat the "whole person."
Despite its proven effectiveness, there's a huge gap in care. In 2023, nearly 54.2 million people in the U.S. aged 12 and older needed substance abuse treatment. And among the 4.8 million people with opioid use disorder, a shockingly low 17% actually received MAT. You can find more of these eye-opening insights on the national state of addiction treatment and recovery from drugabusestatistics.org. This statistic alone highlights just how urgently we need accessible, integrated programs that offer these life-saving medical supports.
Building Strength Through Holistic Practices
So, while medication helps stabilize the brain, holistic support helps you build a life worth protecting. Sustainable recovery is about so much more than just managing symptoms; it’s about creating new sources of strength, connection, and joy. This is where wellness practices become absolutely essential.
Lasting recovery is built on a foundation of healthy habits that nourish the whole person. Integrating these elements into your life provides the emotional and physical strength needed to navigate challenges without turning back to substances.
These aren't just fluffy add-ons. They are core components of a strong recovery plan you'll find in quality programs across Massachusetts.
- Peer Support: There's incredible healing power in connecting with people who just get it. Groups like AA, NA, or SMART Recovery offer a judgment-free zone to share your story and build a sober social network.
- Family Involvement: Addiction and depression don't happen in a vacuum—they affect the entire family. Family therapy can help mend broken trust, teach healthier communication, and create a supportive home environment that is so vital for long-term success.
- Wellness and Nutrition: The connection between what you eat and how you feel is powerful and direct. A balanced diet can genuinely improve your mood and energy, while regular exercise is one of the most proven tools for reducing symptoms of both depression and anxiety.
- Mindfulness and Meditation: These practices are all about learning to stay grounded in the present. Developing the skill to simply observe your thoughts and feelings without immediately reacting to them is a game-changer for managing cravings and overwhelming emotions.
When you combine the stability that medication can provide with the deep-rooted resilience built through these holistic supports, you're not just treating symptoms—you're creating a comprehensive and powerful strategy for a genuinely better life.
Building a Fulfilling Life After Treatment
Getting through a depression and addiction treatment program is a massive accomplishment, but the real journey is just beginning. Now, the work shifts from the structured safety of treatment to the complexities of everyday life. The goal isn't simply to "not use" anymore; it's about building a life that’s so rich and meaningful, you no longer feel the need to escape from it. This is about creating new, healthy routines, finding genuine passions, and leaning on your support system.
Think of it this way: treatment gave you the tools and the blueprint. Now it's time to start construction. You're moving from a defensive position—fighting off old habits—to an offensive one, actively creating a future filled with purpose, connection, and real joy. This is where lasting wellness is built, one day at a time.

Creating Your Aftercare Blueprint
A solid aftercare plan is the scaffolding that holds everything up as you build this new life. It’s not just a suggestion; it’s a critical, personalized strategy for handling the inevitable bumps in the road of long-term recovery. Without this framework, it's dangerously easy to fall back into old patterns when stress or triggers pop up.
Your aftercare plan should be a living, breathing document that changes as you grow. The strongest plans usually rest on a few key pillars:
- Ongoing Therapy: Keeping up with individual or group therapy gives you a dedicated space to work through challenges, sharpen your coping skills, and stay accountable to your goals.
- Structured Support Groups: There’s incredible power in connecting with people who just get it. Groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or SMART Recovery provide a ready-made community for sharing experiences and getting support.
- Alumni Programs: Most good treatment centers in Massachusetts have strong alumni networks. These are fantastic for staying connected to a sober community through social events, special meetings, and a network of people who are on the same path.
Rediscovering Joy and Purpose
A big piece of the recovery puzzle is filling the space that substance use used to occupy with things that actually feed your soul. This is your opportunity to pick up an old hobby you once loved or be brave and try something completely new. Maybe it’s hiking the trails at Blue Hills Reservation, taking a pottery class, or volunteering for a local cause you care about. These activities don't just pass the time; they build self-worth and forge positive, healthy connections.
Building a fulfilling life in recovery means finding healthy sources of dopamine—the brain's reward chemical. Sober hobbies and meaningful connections provide a natural, sustainable sense of pleasure and purpose that substances can never replicate.
Social situations can feel like a minefield at first, and that's okay. It’s perfectly fine to set boundaries—like planning to leave an event early or always having your own non-alcoholic drink in hand. The trick is to be intentional, always putting your well-being first as you learn to navigate the world in this new, healthier way. This isn't about just surviving; it's about truly thriving.
Frequently Asked Questions About Treatment
Stepping onto the path of recovery brings up a lot of practical questions. It's completely normal to feel a bit overwhelmed, but getting clear, straightforward answers can make the whole process feel much less intimidating. We've put together this section to tackle the most common concerns we hear from people looking into depression and addiction treatment right here in Massachusetts.
Why can't I just treat my addiction first?
Simply trying to stop using substances without addressing the underlying depression often doesn't work because the emotional pain that drove the addiction is still there. When that unresolved pain surfaces, the risk of relapse is incredibly high. An integrated approach addresses both issues simultaneously for a stronger, more sustainable recovery.
Is my depression causing my addiction, or is it the other way around?
It’s a classic chicken-and-egg question, and it can go both ways. For some, depression comes first, and substances become a way to cope. For others, heavy substance use actually changes their brain chemistry, triggering a depressive disorder. In the end, it doesn't really matter which came first—both need to be treated together for lasting success.
How do I know if I really need dual diagnosis treatment?
If you find yourself reaching for a substance to numb feelings of sadness, anxiety, or hopelessness, that’s a major red flag. Another tell-tale sign is when you try to quit using, but your mental health takes a nosedive. The only way to know for sure is to get a professional assessment from a qualified treatment facility in Massachusetts, which can give you a clear diagnosis and confirm if a dual diagnosis program is the right path forward.
How long do outpatient programs in Massachusetts usually last?
There's no single answer, as treatment is tailored to your specific needs. However, a Day Treatment Program (PHP) might last several weeks for intensive support. An Intensive Outpatient Program (IOP) often runs for about 8 to 12 weeks. Standard outpatient therapy can continue for months as part of your aftercare plan to ensure you stay on track.
Is treatment for depression and addiction covered by insurance?
Yes, in nearly all cases. Most health insurance plans in Massachusetts are legally required to cover services for mental health and substance use disorders. The specifics, like copays or deductibles, depend on your plan. The best first step is to contact a treatment center’s admissions team—they can verify your benefits and explain your coverage clearly.
How can I help a family member who is in treatment?
Your support is invaluable. The most powerful things you can do are participate in family therapy sessions, educate yourself about co-occurring disorders, and practice setting healthy boundaries. Offer patience and encouragement, and remember that recovery is a long-term process. Consider seeking support for yourself through groups like Al-Anon, which connects you with others in similar situations.

