Deciding to quit drinking is a significant step toward a healthier life, but it can feel overwhelming. This guide breaks down how to quit drinking alcohol into a clear, actionable process, from making the initial decision to building a sober life you love. We'll cover the safest way to stop, what evidence-based treatment looks like, and how to create a solid plan for long-term success, with a special focus on resources available in Massachusetts.
Key Takeaways
- Safety First: Quitting "cold turkey" can be dangerous for heavy drinkers. The first and most critical step is a professional medical assessment to determine if you need supervised detox for safe withdrawal.
- Evidence-Based Treatment is Crucial: Lasting recovery is built on therapies proven to work, such as Cognitive Behavioral Therapy (CBT). Look for treatment that addresses the root causes of drinking, not just the symptoms.
- Flexible Options Exist: You don't have to put your life on hold. Massachusetts outpatient programs like PHP and IOP offer structured, effective treatment that allows you to balance recovery with work and family commitments.
- A Relapse Prevention Plan is Your Roadmap: Long-term sobriety involves identifying personal triggers (emotional, environmental, social) and having a clear, written plan with healthy coping strategies to navigate high-risk situations.
Your First Steps Toward Lasting Sobriety
Making the choice to quit drinking is one of the most powerful decisions you can make for your health and future. It can feel daunting, but you're not swimming against the current. In fact, more people than ever are choosing sobriety.
A recent Gallup survey really puts this into perspective. It found that only 58% of adults in the U.S. had a drink in the past year—the lowest number reported since 1996. This isn't just a random dip; it's part of a larger shift as people become more aware of alcohol's impact on their health. If you're curious, you can learn more about these changing attitudes toward alcohol.
So, what are those first, concrete actions you can take?
- Commit to a 'Quit Date': This isn't just a vague idea. Pick a specific date on the calendar. This makes it real and gives you a clear starting line.
- Know the Risks of Withdrawal: Stopping cold turkey can be dangerous, even life-threatening, for heavy drinkers. It's crucial to understand the signs of withdrawal and recognize when you need to call a doctor or head to a medical facility. Your safety comes first.
- Explore Your Treatment Options: Start looking into what professional, evidence-based help looks like. For folks in Massachusetts, this might mean exploring options like South Shore Recovery Center, which offers structured outpatient programs designed to fit into your real life.
- Start Building Your Support Crew: You can't do this alone. Begin thinking about who in your life—friends, family, or support groups—can be there to cheer you on and hold you accountable.
Why Professional Screening Matters
It's tempting to rely on online quizzes to figure out if your drinking is a problem. They’re quick, private, and can give you a gut check. But they can't replace a real conversation with a professional.
Taking time for honest self-reflection is an important first move. But a professional screening gives you something invaluable: a medically sound diagnosis and a safe, personalized plan to move forward.
It's really important to understand the difference between a self-check and a proper clinical assessment. This table breaks it down.
Self-Assessment vs Professional Screening for Alcohol Use
| Aspect | Self-Assessment (e.g., online quizzes) | Professional Screening (e.g., AUDIT, CAGE) |
|---|---|---|
| Method | A series of standardized questions answered privately online. | A comprehensive evaluation conducted by a licensed clinician or doctor, often including a physical exam and discussion of medical history. |
| Benefits | Completely confidential, easily accessible, and provides a quick, preliminary insight into drinking patterns. | Delivers an accurate medical diagnosis, assesses withdrawal risk, identifies co-occurring mental health conditions, and provides a personalized treatment plan. |
| Limitations | Lacks clinical accuracy, cannot diagnose an alcohol use disorder (AUD), and cannot determine if medical detox is necessary. | Requires an appointment and may feel intimidating, but it is the only way to ensure safety and create an effective, evidence-based recovery strategy. |
While a self-assessment is a good place to start your thinking, a professional screening is what sets you up for a safe and successful recovery. It takes the guesswork out of it and puts expert guidance on your side from day one.
How to Get Through Alcohol Withdrawal Safely
So you’ve decided to stop drinking. That's a huge, life-changing decision. But the next step is just as critical: figuring out how to do it safely.
When your body has become physically dependent on alcohol, quitting cold turkey isn't just about willpower. It can trigger a cascade of withdrawal symptoms, some of which are seriously dangerous. This isn't meant to scare you—it's about giving you the knowledge to protect yourself. Understanding what your body might go through is the first step toward managing it effectively.
What to Expect: The Withdrawal Timeline
Everyone's experience is a bit different, but Alcohol Withdrawal Syndrome (AWS) often follows a rough timeline. Knowing the stages can help you and your loved ones know what to look for and when.
- 6 to 12 hours after the last drink: This is when the early, more familiar symptoms usually kick in. Think anxiety, headaches, an upset stomach, and trouble sleeping. You might also notice hand tremors, what many people call "the shakes."
- 12 to 24 hours: For some, withdrawal can intensify. This is the window where hallucinations—seeing or hearing things that aren't really there—can begin.
- 24 to 48 hours: The risk for seizures is at its peak during this period. This is one of the biggest reasons why having medical support is so crucial.
- 48 to 72 hours: This is when the most severe form of withdrawal, delirium tremens (DTs), can emerge. DTs are a full-blown medical emergency, causing severe confusion, high fever, agitation, and a racing heart.
The thought of withdrawal can feel overwhelming, but a medically supervised detox changes the game. It provides a safe, controlled environment where symptoms are managed around the clock, dramatically lowering the risk of life-threatening complications.
This decision tree helps visualize the critical choice between trying to manage on your own and getting professional help.
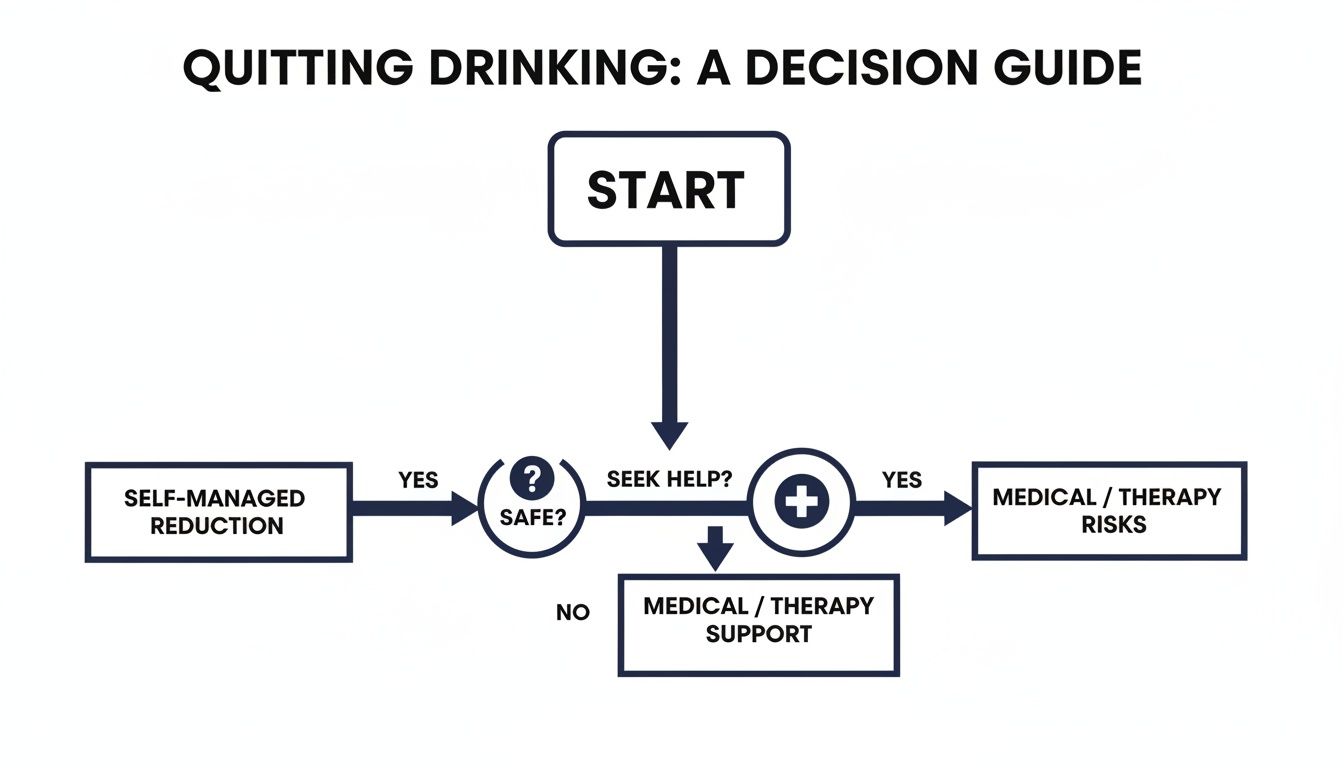
The message is clear: your safety has to come first, and professional guidance is the surest way to get through detox safely.
The Smartest, Safest Choice: Medical Detox
Given the potential for severe, unpredictable symptoms, the safest way to stop drinking for anyone with a physical dependence is almost always through a medical detox program.
In a professional setting, a clinical team can provide medications to make you more comfortable and, most importantly, to prevent dangerous complications like seizures.
For those of us here in Massachusetts, facilities like South Shore Recovery Center offer this exact kind of structured, compassionate care. You get 24/7 medical monitoring from a team that gets it—they understand the science of withdrawal and are there to keep you safe and as comfortable as possible during this really vulnerable time. You can get a much more detailed breakdown of all the alcohol withdrawal symptoms and treatment options to see what that looks like.
Choosing medical detox isn't admitting defeat. It's the opposite. It’s a powerful, proactive step that shows you're serious about building your recovery on the strongest possible foundation. It takes the fear out of the equation and gives you a clear, medically sound plan to navigate the toughest first few days of sobriety.
Finding the Right Evidence-Based Treatment
Once you’re through detox, you’ve won the first battle. Now, the real work of building a sober, fulfilling life can start. This next phase is all about developing the mental and emotional tools you need for the long haul. It's like moving from the ER to a specialist—you’re shifting focus from immediate physical safety to addressing the root causes of drinking.
Recovery isn't a one-size-fits-all journey. What works wonders for one person might not click for another. That's why top-notch treatment centers here in Massachusetts and elsewhere rely on evidence-based therapies. These aren't just good ideas; they're methods proven by solid scientific research to be effective for substance use disorders.
The point of therapy isn’t to erase your past but to empower your future. It's about learning new ways to think, feel, and act so alcohol simply doesn't have a place in your life anymore.
This means your treatment plan should be built around you—your history, your personality, and your specific needs.
Cognitive Behavioral Therapy (CBT): The Foundation of Change
One of the most powerful and widely used approaches is Cognitive Behavioral Therapy (CBT). The core idea behind CBT is actually quite straightforward: our thoughts, feelings, and behaviors are all linked. By learning to spot and challenge the automatic, negative thought patterns that lead you to drink, you can fundamentally change your actions.
For example, maybe a tough day at work triggers the thought, "I'm so stressed out, I deserve a drink to unwind." CBT helps you press pause on that impulse. You learn to recognize it as a high-risk thought and consciously replace it with something more constructive, like, "I'm feeling stressed. A quick walk or calling a friend will help me relax without all the downsides of drinking."
It sounds simple, but over time, this practice actually rewires your brain's default responses. You can get a much more detailed breakdown of how Cognitive Behavioral Therapy works to see just how effective this process can be.
Here's what that process looks like in a real session.

This kind of one-on-one collaboration is where the magic happens. It’s a safe space to dig into your personal triggers and rehearse new coping strategies with an experienced guide.
Expanding the Toolkit with DBT and MAT
While CBT is often the cornerstone of a good treatment plan, other specialized therapies offer crucial tools that can make all the difference.
- Dialectical Behavior Therapy (DBT): Originally designed for borderline personality disorder, DBT has proven incredibly effective for addiction, especially for people who feel overwhelmed by intense emotions. It teaches practical skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. In short, it gives you a concrete playbook for handling tough feelings without reaching for a drink.
- Medication-Assisted Treatment (MAT): This isn't about swapping one substance for another; it's a strategic approach that combines behavioral therapy with FDA-approved medications. For instance, a medication like naltrexone can significantly dial down cravings and block the euphoric effects of alcohol, which makes it much easier to focus on your therapy. Think of it not as a cure-all, but as a powerful ally that helps quiet the physical side of addiction while you do the psychological work.
The data backs this up. Research shows that Cognitive Behavioral Therapy can lead to sobriety rates of 40-60% at the one-year mark. When you add medications like naltrexone into the mix, you can cut the risk of relapse by another 20-50%.
Finding Your Fit in Massachusetts
Here on the South Shore, the best treatment programs understand that you can't be forced into a one-size-fits-all box. A good program will create a truly personalized plan for you, often blending elements of CBT, DBT, and MAT. This integrated approach is delivered through different levels of care, like Day Treatment or Intensive Outpatient Programs, depending on what your life requires.
The goal is to ensure you’re not just stopping a behavior, but actively building a strong, resilient foundation for a life you genuinely enjoy—free from alcohol. It all comes down to finding that perfect combination of tools, support, and structure that works for you.
How Massachusetts Outpatient Programs Support Recovery
For a lot of people, the thought of putting life on pause for 30, 60, or 90 days to check into an inpatient facility just isn't an option. Work, family, and other obligations don't simply disappear. The great news is, you don’t have to. Massachusetts has a strong network of outpatient programs that deliver structured, evidence-based care while letting you stay connected to your life at home.
The whole point of outpatient treatment is to weave recovery into your real world from the very beginning. It’s built to be flexible enough for your schedule but intensive enough to provide the clinical support you need. This approach helps you build resilience right where it counts—in the exact environment you'll be living in for the long haul.
Understanding Different Levels of Outpatient Care
Not all outpatient programs are created equal. They exist on a spectrum of intensity, designed to meet you exactly where you are in your recovery. The main structures you’ll encounter are Day Treatment Programs (also called Partial Hospitalization or PHP) and Intensive Outpatient Programs (IOP).
To make sense of these options, it helps to see how they compare in terms of time commitment and who they're designed for.
Levels of Outpatient Care in Massachusetts
| Program Level | Typical Weekly Commitment | Best Suited For |
|---|---|---|
| Day Treatment (PHP) | 25-30 hours (5 days/week, ~6 hours/day) | Individuals needing significant structure, often as a step-down from inpatient care or detox. |
| Intensive Outpatient (IOP) | 9-15 hours (3-5 days/week, ~3 hours/day) | People with a stable home life who need to balance treatment with work, school, or family responsibilities. |
| Outpatient (OP) | 1-3 hours (1-2 days/week) | Those who have completed a higher level of care and are focused on maintaining long-term recovery. |
This tiered system ensures you get the right amount of support without being overwhelmed or underserved, allowing for a smoother transition as you gain more confidence in your sobriety.
What Does a Typical Week Look Like?
Let's make this real. Imagine Sarah, a teacher from a town near Plymouth. After finishing medical detox, she enrolls in a Day Treatment Program (PHP). Her week is structured: daily morning group therapy on relapse prevention, followed by a one-on-one session with her therapist to tackle her anxiety. In the afternoon, she joins a skills group to learn mindfulness before heading home to her family for dinner.
Or think about David, a construction worker who can’t afford to lose his job. An Intensive Outpatient Program (IOP) is a perfect fit. He works his regular shift and then attends therapy sessions three evenings a week. His treatment plan includes group counseling with guys who get what he's going through, family therapy with his wife, and regular check-ins to manage his medication-assisted treatment (MAT).
In both cases, you can see how Massachusetts outpatient alcohol treatment molds itself to the person’s life, not the other way around. That flexibility is one of its biggest strengths.
Don't mistake outpatient care for a "lighter" version of treatment. It's a different, highly effective model that empowers you to use coping skills in real-time, turning daily challenges into growth opportunities with the immediate support of your clinical team.
Making It Work For You
Considering this path? Here are a few things I've seen make all the difference for people who succeed in outpatient programs:
- Structure is Your Friend: Active addiction often brings chaos. Outpatient programs restore a predictable, healthy routine, creating the accountability and stability that recovery thrives on.
- Find Your People: You are not in this alone. Group therapy is powerful because it connects you with others who genuinely understand the struggle, creating a sense of community that is hard to find anywhere else.
- Practice in the Real World: You get to immediately apply what you learn. A tough conversation at work or a family dinner becomes a chance to practice new coping skills, building real confidence.
- Flexibility for the Long Haul: By letting you stay engaged with your life, outpatient care makes recovery a sustainable, integrated part of who you are, rather than something you do while you're away at a facility.
Building a Practical Relapse Prevention Plan
Long-term sobriety isn’t about white-knuckling it through cravings. It’s about having a smart, practical game plan for the tough moments. A relapse prevention plan is exactly that—your personal roadmap for navigating the inevitable challenges that recovery throws your way.
Think of it as preparing for a storm. You don’t wait for the downpour to start looking for your umbrella. You map out the potential risks ahead of time and have your defenses ready. This plan gives you structure and a clear path forward when a trigger hits, taking the guesswork out of a high-pressure situation.
Identify Your Personal Triggers
First things first: you have to get brutally honest about what makes you want to drink. Triggers are deeply personal, but they usually fall into a few common buckets. The more specific you can be here, the more effective your plan will be.
- Emotional Triggers: These are the feelings your brain has learned to "solve" with alcohol. Maybe it’s the crushing stress after a long day at work, the quiet loneliness of a weekend evening, or the flash of anger after a fight with your partner.
- Environmental Triggers: Think about the people, places, and even sensations you connect with drinking. This could be a specific bar in Boston, a certain group of friends, the sound of a can cracking open, or even just driving past the same liquor store on your commute home.
- Social Triggers: These are the situations where you feel the pressure—spoken or unspoken—to drink. Holiday parties are a big one, as are after-work happy hours, summer barbecues, or watching a Patriots game with your buddies.
Getting these down on paper is a powerful first step.

This is the core of relapse prevention: turning abstract fears into a concrete, written strategy you can pull out in a moment of crisis.
Develop Healthy Coping Skills
Knowing your triggers is half the battle. The other half is deciding what you’ll do instead of drinking when they show up. This is where you build a brand-new toolkit of healthy coping mechanisms. The idea is to have several options ready to go, so you can pick the one that fits the situation.
Your coping skills are your new default responses. The more you practice them, the more automatic they become, slowly but surely replacing the old, ingrained habit of reaching for a drink.
It helps to have a written list you can glance at when you feel a craving coming on. It might include things like:
- Call a Support Person: Have a short list of 2-3 trusted people—a sponsor, a sober friend, a supportive family member—you can call or text anytime.
- Practice Mindfulness: A simple breathing exercise can work wonders. Inhale for four seconds, hold for four, and exhale for six. Do this 5-10 times to calm your nervous system right down.
- Change Your Environment: If you’re at home feeling antsy, get up and go for a walk. If you’re at a party that’s becoming overwhelming, step outside for some fresh air or just make your exit.
- Engage in a Hobby: Pick up your guitar, work on a puzzle, head to the gym, or do anything that fully occupies your hands and your mind.
Build Your Sober Support Network
Recovery is not a solo mission. A strong support system is one of the most reliable predictors of long-term success. This is your crew—the people who get it and actively support your decision to live alcohol-free.
This network should ideally be a mix of professional and personal support. For those in Massachusetts, this could mean continuing with an outpatient group at a center like South Shore Recovery, finding local AA meetings that feel right, and staying connected with sober friends you met in treatment.
It’s also crucial to have honest conversations with family and close friends about how they can best help you. This might mean asking them not to drink around you for a while, especially in the early days.
Have a Plan for High-Risk Situations
Finally, walk yourself through the specific, high-risk scenarios you know are coming. Don't wait until you're in the moment to try and figure it out.
-
Scenario: You’re out to dinner with coworkers, and the server comes to take drink orders.
-
Your Plan: Have your non-alcoholic order ready before you even sit down. "I'll have a club soda with lime, thanks." Saying it quickly and confidently signals that it's not up for debate.
-
Scenario: An old friend who doesn’t know you’ve quit texts, "Let's hit the bar tonight!"
-
Your Plan: Practice a polite but firm response. "Thanks for thinking of me, but I’m not drinking these days. How about we grab coffee next week instead?"
By planning your response, you remove the element of surprise and keep yourself in the driver's seat. Your relapse prevention plan isn't set in stone—it’s a living guide. Revisit it, tweak it, and let it grow with you as you get stronger in your recovery.
Frequently Asked Questions About Quitting Alcohol
When you're thinking about how to stop drinking, a million questions can start swirling around. That's completely normal. Getting solid, straight-up answers is one of the best ways to quiet the noise and figure out your next step.

What is the very first thing I should do?
Talk to a healthcare professional. Period. They can look at your specific situation, figure out your risk level for withdrawal, and guide you on the safest way to cut back or stop completely. This is the most critical first step.
Is it safe to detox from alcohol at home?
The short answer is no. While the thought of detoxing in the comfort of your own home is appealing, it's incredibly dangerous and can even be fatal. Alcohol withdrawal can trigger severe, life-threatening symptoms like seizures or delirium tremens (the "DTs"). For anyone with a history of heavy drinking, a supervised medical detox is always the safest route.
How long is this recovery process going to take?
There's no finish line here—recovery is a lifelong journey. The first phase is the most intense, with detox lasting anywhere from a few days to a couple of weeks, often followed by a structured treatment program for 30, 60, or 90 days. The goal of treatment isn't just to get you sober; it's to equip you with the skills, mindset, and support system you need to stay sober for the long haul.
What happens if I relapse?
First, take a deep breath. A relapse is not a failure—it's a common part of the recovery journey for many people. It's a sign that your current strategy needs a tune-up, not that you should give up. The most critical thing you can do is reach out for help immediately. Call your therapist, your sponsor, or a trusted local support group in Massachusetts. Don't let shame keep you isolated.
How do I find local help in Massachusetts?
A simple search for "outpatient addiction treatment Massachusetts" is a great start. You can also contact centers like South Shore Recovery Center directly to ask questions. Don't forget your primary care doctor—they are an excellent resource for referrals to local programs and specialists who can help.
